5 Lifestyle Habits To Improve your Parkinson's Disease
Who is Dr. Mischley?
Dr. Mischley’s work is focused on identifying nutritional requirements unique to individuals with neurodegenerative diseases. She has conducted research on coenzyme Q10, lithium, and glutathione (GSH) deficiency in the setting of Parkinson’s Disease (PD). As a clinical trialist, she is interested in determining whether intranasal GSH boosts brain GSH and potentially improves PD outcomes . She developed the PRO-PD rating scale and is developing a PD screening tool, ParK-9; using dogs to identify the scent of PD from ear wax. She is principal investigator of the “CAM Care in PD” study which is designed to identify the relationship between lifestyle choices and risk of PD progression. As a naturopathic physician, she maintains a clinical practice at Seattle Integrative Medicine and conducts research in collaboration with the University of Washington and Bastyr University.
We sat down with Dr. Mischley to pick her brain and to better understand the direction her research is taking. She is passionate to help those with PD and although her data is preliminary it is a really interesting discussion.
Watch Dr. Subramanian interview Dr. Mischley about patient centered outcomes and research
1. Why is it important to focus on patient centered
outcomes?
When researchers and clinical providers are asked to describe PD, they’ll often start out by talking about the motor symptoms— the tremor, the rigidity and the slowness. But when we asked patients to describe the disease, they emphasized fatigue, muscle pain, impaired sleep, sexual dysfunction, apathy, etc. The scientific community needs to take a step back and and to do a better job of listening to patients. Patient-reported outcomes are measurements made based on the opinion of the patient, not the judgement of the clinician. The lack of objective measures (things that can be counted or measured exactly) makes a lot of scientists uncomfortable, but the truth is that the patent’s opinion is the gold standard— There is no tool that is more capable of rating a patient’s fatigue, apathy, or anxiety than the patient him or herself. I’m passionate to advocate that researchers incorporating patient-reported outcomes and measures of quality of life into all of their studies.
2. What should I be eating?
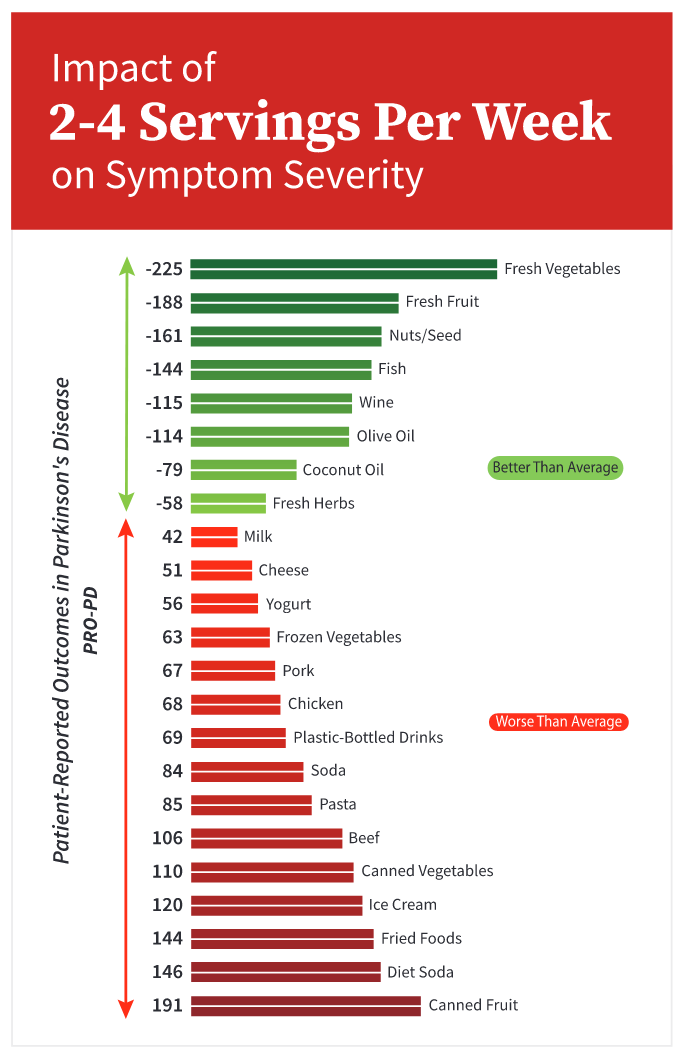
Over the past 7 years we’ve surveyed thousands of people with Parkinson’s to find out whether the people with more rapidly progressing disease were eating different foods than those with slowly and/or non-progressive disease. Here’s what we learned: On the graph above, the foods in green were associated with statistically fewer symptoms over time. Fresh vegetables, fresh fruit, nuts & seeds, non-fried fish, wine, olive oil, coconut oil, & fresh herbs. The more of the foods people ate from the bottom of the graph, the faster the accumulation of PD symptoms over time. Canned fruits, canned vegetables, fried food, soda/ diet soda, ice cream yogurt, cheese, milk, beef, chicken, pork, pasta, frozen vegetables and drinking from plastic bottles.
If you stop eating the foods in red and load up on the foods in green, will it improve your disease? We don’t know— that study hasn’t been done. Research efforts are underway to determine whether changing your diet will result in improved outcomes over time. This data is preliminary and drawn from our experience.
3.Do I have to eat organic foods?
It’s not all about particular foods. We also have observed in our data that people who cook most of their own meals and routinely cook for others seem to be doing better than people who eat out more often. We have some data to suggest that people that go out of their way to attempt to buy local, organically sourced food also seem to be accumulating fewer symptoms over time. Perhaps one of the most important findings from our research has been the impact of food scarcity on PD progression— the single biggest predictor of PD progression we’ve identified so far is the inability to afford groceries. Before seeing these data, I personally thought of income as something that could allow/ prevent access to good health care. Now, I’m spending a lot more time considering whether the chronic stress associated with poverty or the nutritional deficiencies that come from eating cheap, highly-processed food might be contributing to disease. This is just my hypothesis and it is something I am interested in pursuing.
4. What type of exercise should I be doing?
Of the choices listed above, running and yoga were the two forms of exercise associated with the fewest symptoms over time in our dataset. I found this particularly interesting because they are so different— one is highly aerobic, increasing body temperature and heart rate, while yoga tends to emphasize mindfulness, breath, balance, and a balance of strength and flexibility. We’ve just launched the 2020 CAM Care PD survey, which has a much greater emphasis on different types of exercise, with a focus on duration and intensity. This data should be interpreted as preliminary. We know exercise is good in Parkinson’s and I expect we will learn over the next 5-10 years if one form may have advantages over another.
5. How many days a week and for how long should l
be exercising?
In this study, we asked people how often they did at least 30 min of exercise. We saw a clear dose-response curve- the more days per week people exercised, the fewer symptoms they reported over time. Especially relevant to patients is that the first two days per week of exercise did not seem to translate to slower progression over time. At three days per week, and each day after, the impact on symptoms got increasingly better. This data was of course from a survey, but the theme of more exercise is better seemed to emerge. We are going to look at this question more carefully in the future.
6. What other lifestyle habits may be important
especially given COVID-19?
Dr. Laurie Mischley along with Dr. Indu Subramanian and Josh Farahnik performed a study looking at a large cohort of persons with Parkinson’s (PWP). Individuals who responded “True” to the statement, “I am lonely” reported approximately 55% greater PD symptom severity over time. The higher the quality of life score, the more likely the participant was to say they had a lot of friends or the more likely it was that they were partnered or married. The lower the quality of life score, the more likely they were to report being lonely. We found that being lonely was as bad for a PWP as the beneficial effects of exercising 7 days a week for 30 min per day. Lonely PWPs reported greater symptom severity for all 33 symptoms measured. Not unexpectedly, the greatest discrepancies between lonely and non-lonely individuals were found with social withdrawal/loss of interest, motivation/initiative, depression, and anxiety. This data was highlighted as a top abstract at the Movement Disorders Society Congress 2020. It is currently in press at NaturePJ Parkinson’s Disease Journal. We plan to confirm the data with future studies and to better understand how we can intervene to improve quality of life and to address lonliness.
By Jonny Acheson
6. How can I get more involved in this type of
research?
The Complementary and Alternative Medicine in PD (CAM Care PD) study was designed to identify modifiable variables associated with the rate of patient-reported PD severity and progression. There were 1,527 participants with PD available for this analysis. Our study was a prospective, observational internet-based study that was designed to identify modifiable lifestyle variables associated with the accumulation of patient-reported symptoms over time. We are trying to enroll as many patients as possible! Currently we are studying the impact of COVID-19 on how patients are doing with their quality of life and their PD. We would love to have you be part of this study. Toward the end of this year we will be updating all the analyses in preparation for the 2021 report— now is the time to enroll! Everything you need to get started can be found at this weblink and these addresses:
Additional references: www.LivingHealthyWithParkinsons.com
Original publication discussing study methodology: https://www.hindawi.com/journals/omcl/2017/6405278
This blog is brought to you by Michael S. Okun and Indu Subramanian.
To read more books and articles by Michael S. Okun MD check Twitter @MichaelOkun and these websites with blogs and information on his books and http://parkinsonsecrets.com/ #EndingPD #ParkinsonPACT #Parkinsonsecrets and https://www.tourettetreatment.com/
He also serves as the Medical Director for the Parkinson’s Foundation.
To see more on Dr. Indu Subramanian she does live interviews of experts in Parkinson’s for the PMD Alliance