Do you know the 5 standards you should demand if hospitalized with Parkinson's?
By Michael S. Okun
The Parkinson’s Foundation first developed the aware in care kit and this morphed into an important free book for the field, the Hospital Safety Guide.
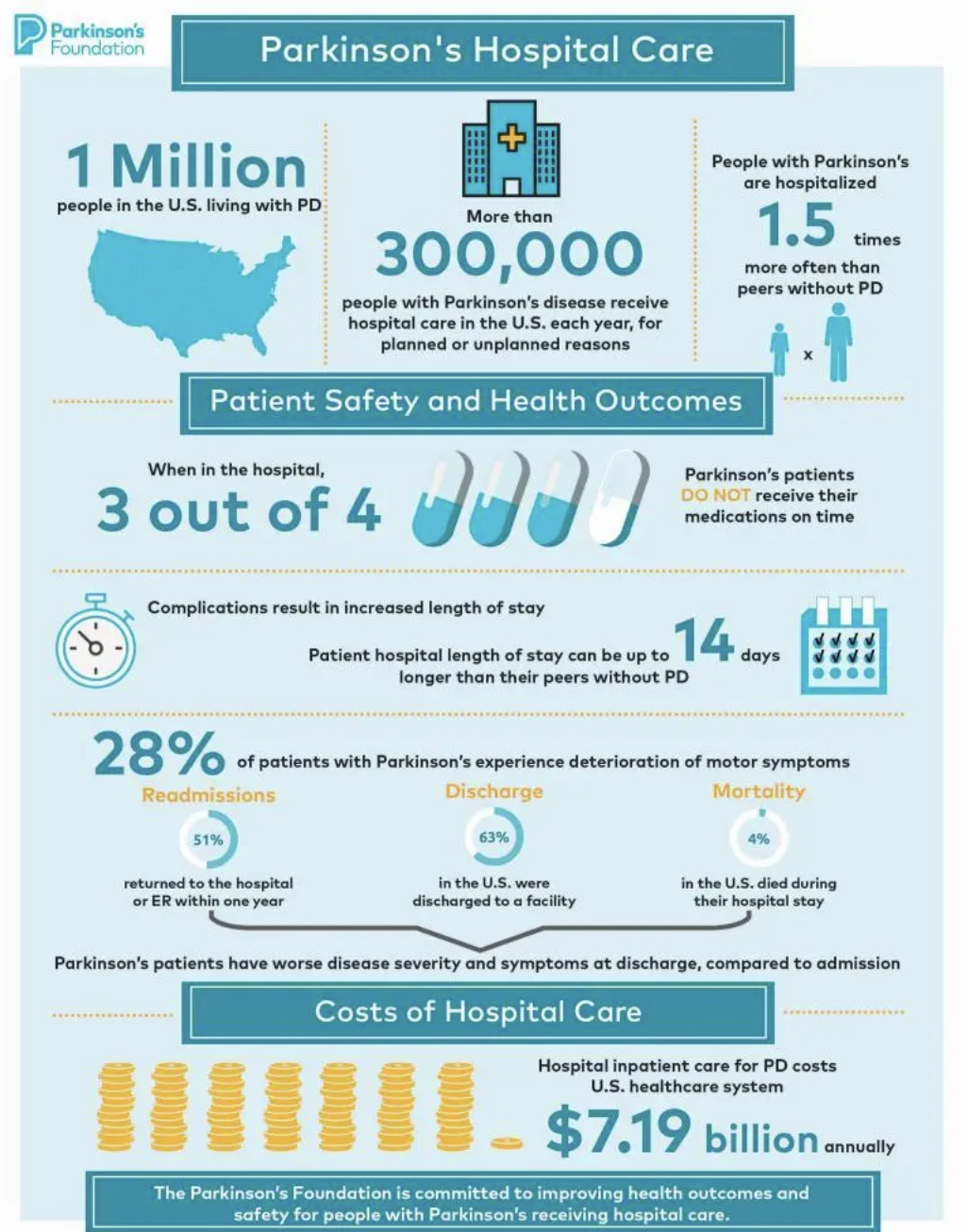
The hospital is not a safe place if you have Parkinson’s disease. There is a 1 in 3 chance every year that if you have Parkinson’s, you will be hospitalized. A reasonable expectation would be that following hospitalization you would be rapidly discharged to home, and that your Parkinson’s symptoms would not worsen. The reality is far from where you might think it is. A large group of centers of excellence in the Parkinson’s Foundation network have been publishing papers and creating practical guidelines, kits and most recently a free book on hospitalization safety. Most recently, they have published an important commentary in the Joint Commission Journal on Quality and Safety. The authors are advocating that we insist on implementation and enforcement of 5 hospitalization care standards. It is important that we raise awareness and implement a proactive plan for Parkinson’s disease hospitalizations.
A person gets diagnosed with Parkinson’s disease every 6 minutes.
Why do we care about preventing harm in hospitalized Parkinson’s folks?
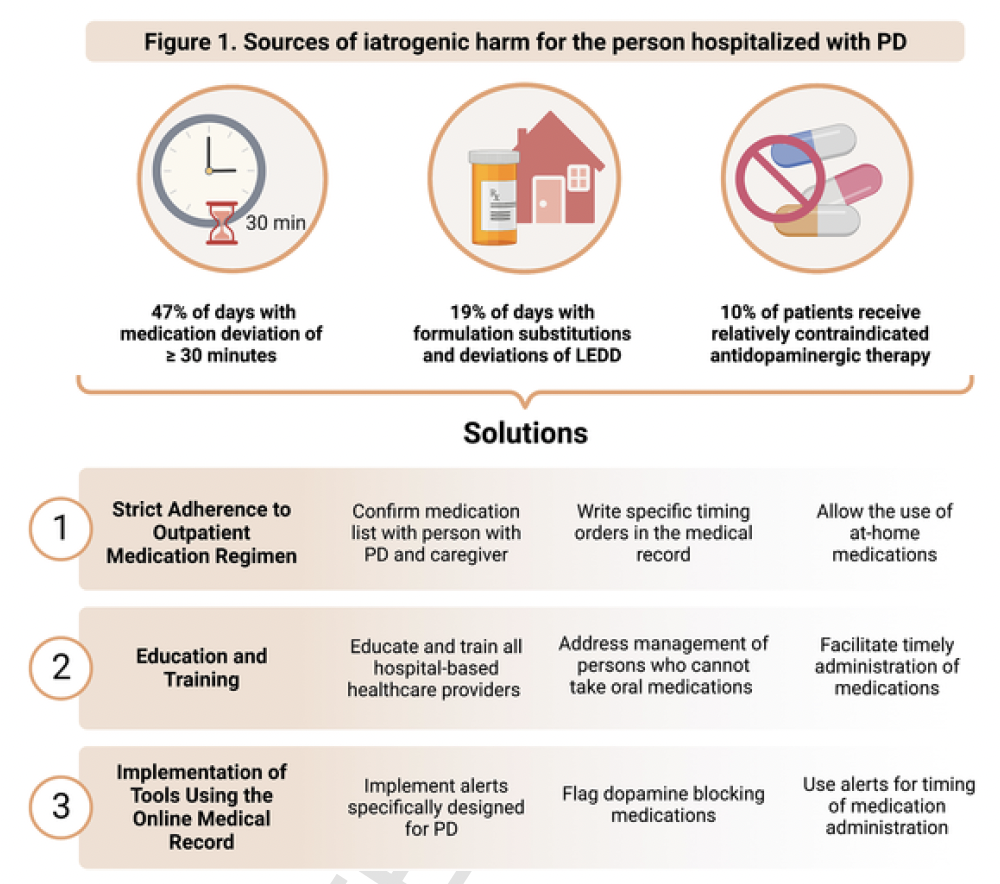
There are disproportionate rates of preventable and unintended harm in the acute care hospital setting, regardless of the reason for admission. The adverse outcomes may include:
Deterioration of motor symptoms in 28%
Increased length of stay up to 14 days longer
Higher rates of delirium in 11%-60%
Higher mortality (death) with a mortality ratio as high as 3.8 among Parkinson’s patients compared to controls
Parkinson’s folks are more likely to be readmitted within one year of discharge in 51%
The person would be more likely to be discharged to another facility, rather than to home in 62.9%
A recent editorial in Parkinsonism and Related Disorders offered some useful tips for Parkinson’s hospitalization.
Why does the Joint Commission care so much about the hospitalized Parkinson’s person?
First, who is the joint commission? The Joint Commission accredits and certifies more than 22,000 health care organizations and programs in the United States. This includes hospitals .
There is increasing pressure from policymakers, accrediting bodies, and regulatory agencies to improve patient safety and quality.
Safety and quality are disproportionately impacted in Parkinson’s disease.
The Centers for Medicare & Medicaid Services and The Joint Commission have set quality goals for readmissions.
Falls are common in Parkinson’s, and injuries are tracked as sentinel events. These are higher in Parkinson’s.
Do you know the shocking facts about Parkinson’s hospitalization?
What are the current Parkinson’s Foundation hospital care recommendations?
The Parkinson’s Foundation published (2023) the Parkinson’s Foundation Hospital Care Recommendations.
There is now a systematic quality improvement framework which can be applied to improve hospital care.
What are the 5 recommendations you should insist on if hospitalized with Parkinson’s?
There are 5 hospital care standards that I believe we must be met to avoid preventable harm in Parkinson’s. These are recommended by the Parkinson’s Foundation.
1. All Parkinson’s disease medications are ordered in a custom fashion according to your at-home regimen. Deviations from stable at-home schedules are known to increase the risk of motor deterioration, given the short half-lives of dopaminergic medications. Ensuring that clinicians order inpatient Parkinson’s disease medications in a custom fashion will ensure medications are received ‘on time every time.’ This practice has the potential to reduce the length of stay.
2. All Parkinson’s medications are administered within ± 15 min of your at-home regimen. This should be accomplished in the hospital 100% of the time. Early or delayed medication administration, even within 30 or 60 minutes of at-home schedules can result in negative outcomes. While the evidence is limited on the precise window to prevent harm, the window narrows as the disease continues to progress and dosing becomes more frequent.
3. Harmful medication events are eliminated. Focus should be placed on dopamine-blocking medications, pain medications, and sedatives. Commonly contraindicated (do not take) medications like haloperidol, metoclopramide, and prochlorperazine must be avoided. There are also medications that are not contraindicated by definition or flagged in common electronic medical record alerts, but can also be harmful.
4. Mobilize 3 times a day if clinically appropriate and under professional supervision. There is limited evidence on the exact amount or type of mobilization required to prevent harm. However, there is consensus that early mobilization as critical to avoiding complications.
5. Screening for dysphagia (swallowing) within 24 hours. This can minimize the risk of aspiration pneumonia. There is a high risk of mortality related to aspiration pneumonia in the hospital (25%).
How can hospitals and groups implement these changes?
The aware in care kit was the precursor to the Parkinson Hospitalization safety guide.
The new guidelines suggest use of an implementation management system. This recommendation is for the clinicians and hospital administration and not for the person with Parkinson’s.
The first step is preparatory, convening a multidisciplinary working group and clinical quality champions to drive change and to use the electronic medical record.
The second step determines the initial scale of implementation (e.g., within a single unit, a single hospital, or multiple hospitals in a health system or hospital of a health system) and also the tactics.
The final step should expand implementation beyond initial tactics.
What are some tips or tactics you could suggest to your doctor or health care provider for improvement and implementation in the hospital?
Suggest for them to order medications in a custom fashion
Determine your at-home regimen and consequences of delayed medication upon admission as part of the medication reconciliation process
Encourage them to use a custom input for medications to align with at-home regimens, rather than use default medication schedules
Encourage them to improve hospital-wide awareness of preventable harm through aggressive programs.
Advocate for them to administer medications within ± 15 min of patients’ at-home regimen
Make sure they implement data collection and review mechanisms that track and assess the discrepancy between your at-home regimen and in-hospital medication administration
Encourage them to implement standard processes for reducing delays in medication administration.
Remind them to avoid unnecessary orders on not take anything by mouth (NPO)
Discuss and identify with your health care provider potentially contraindicated or potentially harmful medications.
Make sure they are using electronic health records based safeguard to avoid the prescription and administration of contraindicated medications
Remind them to avoid inappropriate treatment of psychosis, confusion, or delirium with contraindicated antipsychotics
Remind them to avoid contraindicated nausea/GI medications prescribed as part of standard postoperative care
Remind them to avoid unnecessary medication substitutions
Ask them to mobilize you 3 times a day in the hospital
Ask them to provide you with opportunities fto move safely and frequently in the hospital environment
Ask them to order Physical Therapy (PT) and occupational therapy (OT) when you are in the hospital.
Ask them to include you in any opportunities for communication and collaboration about improving your mobility in the hospital.
Make sure they screen you for dysphagia within 24 hours
make sure they have established and offered you a standard protocol for screening of your swallowing abilities
Make sure they have a protocol for minimizing the risk of you getting aspiration pneumonia in the hospital
Make sure they establish a protocol for medication management for you if you have swallowing challenges, and make sure the medication regimen is as close as possible to your home regimen
Does the use of custom orders in the chart matter?
Researchers from Hackensack University Medical Center published a study in December 2023 that evaluated over 31,000 PD medication orders and determined that custom orders were more likely to result in timely medication administration when compared to non-custom orders.
Researchers from the University of Rochester published a study evaluating the impact of a best practice advisory (BPA) on contraindicated medications and determined that both contraindicated (those medications you should not get) medication orders and administrations were reduced after implementation.
Researchers from Cleveland Clinic published findings from a study examining the impact of changes in dosing and timing of medications from the stable home regimen. They showed a significant increase in length of stay, readmission, and death. This group of authors reminded us of the importance of utilizing drug-disease interaction alerts.
Finally there is a Parkinson’s Foundation Hospital Care Learning Collaborative with two dozen hospitals and health systems of varying size and complexity committed to sharing, implementing, testing, and refining best practices. If your hospital isn’t part of it, you can suggest to your healthcare providers to either join or subscribe to the findings.
What is the bottom-line take home message
If you are planning a hospitalization or end up with an unplanned hospitalization then remember to insist on these 5 items:
1. Make sure your healthcare providers order medications in a custom fashion using the at-home regimen.
2. Make sure your providers administer medications within ± 15 min of a persons’ at-home regimen.
3. Make sure your providers DO NOT use dopamine-blocking medications, pain medications, and sedatives which can worsen your Parkinson’s.
4. Make sure they mobilize you 3 times a day in the hospital.
5. Make sure they screen for swallowing within 24 hours of the hospitalization.
Now close your eyes and imagine if you were able to implement these 5 things, how much would we could improve your Parkinson’s hospitalization experience. A TON!
Dr. Michael Okun is coauthor of the books the Parkinson’s Plan and Ending Parkinson’s. His blogs can be found at PDplan.org and parkinsonsecrets.org
Jonny Acheson is the website artist. He is also a doctor and a person with Parkinson’s disease.
Selected references:
Azmi H, Walter BL, Brooks A, Richard IH, Amodeo K, Okun MS. Editorial: Hospitalization and Parkinson's disease: safety, quality and outcomes. Front Aging Neurosci. 2024 Apr 4;16:1398947. doi: 10.3389/fnagi.2024.1398947. PMID: 38638192; PMCID: PMC11024459.
Veilleux Carpentier A, Salloum RG, Okun MS. Practical proactive and preventative Parkinson's disease strategies for management in the hospital setting. Parkinsonism Relat Disord. 2023 Aug;113:105515. doi: 10.1016/j.parkreldis.2023.105515. Epub 2023 Jul 4. PMID: 37453869.
Shahgholi L, De Jesus S, Wu SS, Pei Q, Hassan A, Armstrong MJ, Martinez-Ramirez D, Schmidt P, Okun MS. Hospitalization and rehospitalization in Parkinson disease patients: Data from the National Parkinson Foundation Centers of Excellence. PLoS One. 2017 Jul 6;12(7):e0180425. doi: 10.1371/journal.pone.0180425. PMID: 28683150; PMCID: PMC5500337.
Zeldenrust F, Lidstone S, Wu S, Okun MS, Cubillos F, Beck J, Davis T, Lyons K, Nelson E, Rafferty M, Schmidt P, Dai Y, Marras C. Variations in hospitalization rates across Parkinson's Foundation Centers of Excellence. Parkinsonism Relat Disord. 2020 Dec;81:123-128. doi: 10.1016/j.parkreldis.2020.09.006. Epub 2020 Oct 3. PMID: 33120073.
Chou KL, Zamudio J, Schmidt P, Price CC, Parashos SA, Bloem BR, Lyons KE, Christine CW, Pahwa R, Bodis-Wollner I, Oertel WH, Suchowersky O, Aminoff MJ, Malaty IA, Friedman JH, Okun MS. Hospitalization in Parkinson disease: a survey of National Parkinson Foundation Centers. Parkinsonism Relat Disord. 2011 Jul;17(6):440-5. doi: 10.1016/j.parkreldis.2011.03.002. Epub 2011 Apr 1. PMID: 21458353; PMCID: PMC3895941.
Hassan A, Wu SS, Schmidt P, Dai Y, Simuni T, Giladi N, Bloem BR, Malaty IA, Okun MS; NPF-QII Investigators. High rates and the risk factors for emergency room visits and hospitalization in Parkinson's disease. Parkinsonism Relat Disord. 2013 Nov;19(11):949-54. doi: 10.1016/j.parkreldis.2013.06.006. Epub 2013 Jul 5. PMID: 23835430.
Aminoff MJ, Christine CW, Friedman JH, Chou KL, Lyons KE, Pahwa R, Bloem BR, Parashos SA, Price CC, Malaty IA, Iansek R, Bodis-Wollner I, Suchowersky O, Oertel WH, Zamudio J, Oberdorf J, Schmidt P, Okun MS; National Parkinson Foundation Working Group on Hospitalization in Parkinson's Disease. Management of the hospitalized patient with Parkinson's disease: current state of the field and need for guidelines. Parkinsonism Relat Disord. 2011 Mar;17(3):139-45. doi: 10.1016/j.parkreldis.2010.11.009. Epub 2010 Dec 14. PMID: 21159538; PMCID: PMC3070297.
Yu JRT, Sonneborn C, Hogue O, Ghosh D, Brooks A, Liao J, Fernandez HH, Shaffer S, Sperling SA, Walter BL. Establishing a framework for quality of inpatient care for Parkinson's disease: A study on inpatient medication administration. Parkinsonism Relat Disord. 2023 Aug;113:105491. doi: 10.1016/j.parkreldis.2023.105491. Epub 2023 Jul 7. PMID: 37495500.
Azmi H, Cocoziello L, Harvey R, McGee M, Desai N, Thomas J, Jacob B, Rocco A, Keating K, Thomas FP. Development of a Joint Commission Disease-Specific Care Certification Program for Parkinson Disease in an Acute Care Hospital. J Neurosci Nurs. 2019 Dec;51(6):313-319. doi: 10.1097/JNN.0000000000000472. PMID: 31626076.
Bobek M, Pascarelli P, Cocoziello L, Azmi H. Utilizing the Nursing Professional Development Model to create and sustain nursing education aimed at improving the care of patients with Parkinson's Disease in the hospital. Front Med (Lausanne). 2024 Jan 24;10:1275970. doi: 10.3389/fmed.2023.1275970. PMID: 38327273; PMCID: PMC10847593.
Azmi H, Cocoziello L, Nyirenda T, Douglas C, Jacob B, Thomas J, Cricco D, Finnerty G, Sommer K, Rocco A, Thomas R, Roth P, Thomas FP. Adherence to a strict medication protocol can reduce length of stay in hospitalized patients with Parkinson's Disease. Clin Park Relat Disord. 2020 Oct 16;3:100076. doi: 10.1016/j.prdoa.2020.100076. PMID: 34316654; PMCID: PMC8298768.