Experiencing Menopause with Parkinson’s? Consider Yoga.
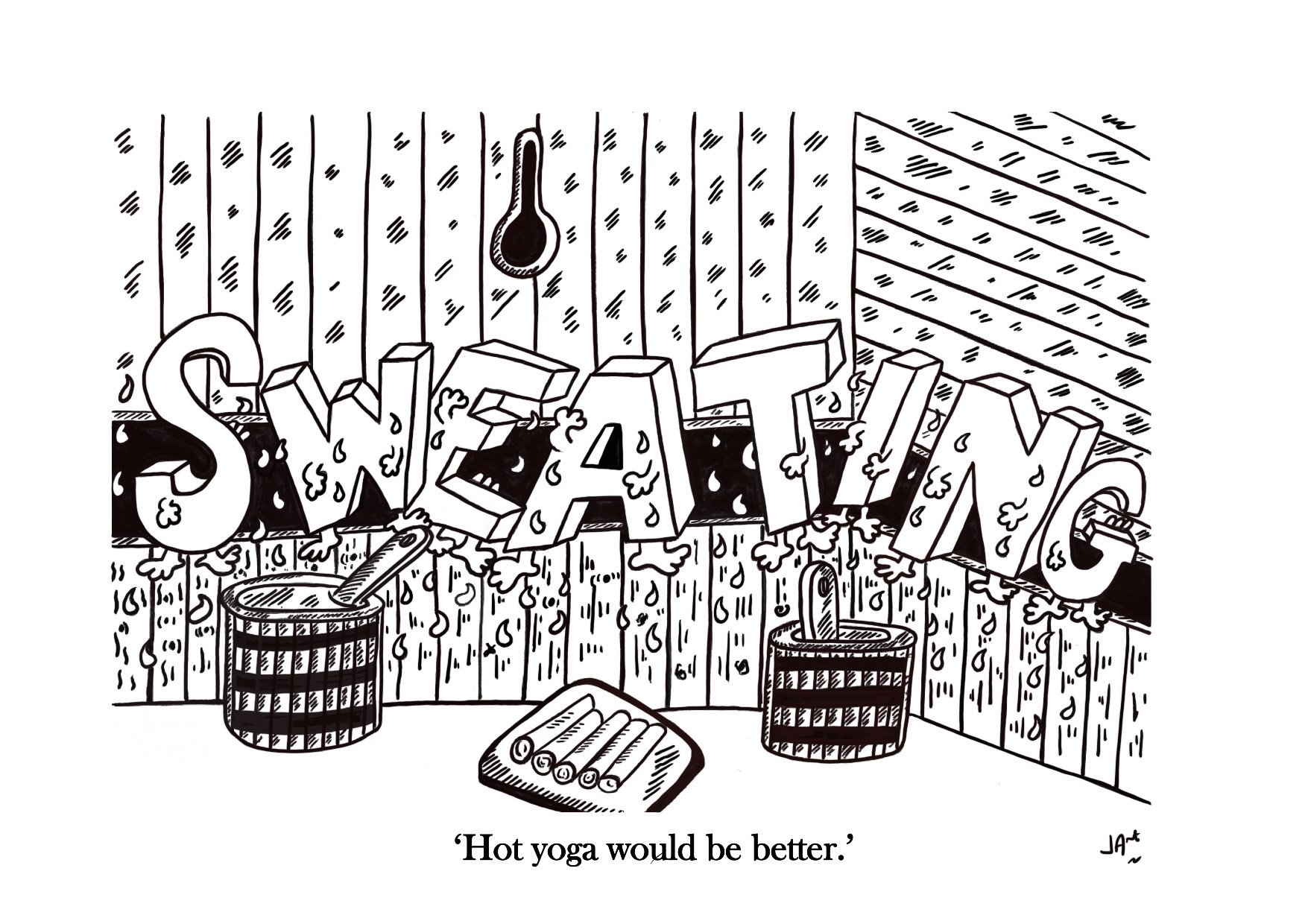
Great pic by our website artist Jonny Acheson.
This month one of our website editors Indu Subramanian tackles two important topics in Parkinson’s; yoga and post-menopausal symptoms. One challenge we frequently under-appreciate in women is that in addition to non-motor Parkinson’s symptoms, they may also experience post-menopausal symptoms. Dr. Subramanian takes us on a journey to explore alternatives and strategies with Dr. Andrew McGonigle.
What is the overlap between menopause symptoms and non-motor or motor Parkinson’s disease symptoms?
The Mayo clinic has summarized the 10 common menopause symptoms as:
Irregular periods
Vaginal dryness
Hot flashes
Chills
Night sweats
Sleep problems
Mood changes
Weight gain and slowed metabolism
Thinning hair and dry skin
Loss of breast fullnes
We have highlighted that half (5/10) are symptoms which can occur without menopause in Parkinson’s. Experts treating Parkinson’s, in general, believe that stress, anxiety, sleep deprivation and menopause can worsen Parkinson’s symptoms.
Why yoga for Parkinson’s and menopause?
There is a growing body of evidence for many exercises benefiting Parkinson’s disease. Kwok et al in JAMA Neurology in 2019 showed that “among patients with mild-to-moderate PD, the mindfulness yoga program was found to be as effective as stretching and resistance training in improving motor dysfunction and mobility, with the additional benefits of a reduction in anxiety and depressive symptoms and an increase in spiritual well-being and health related quality of life.
So why yoga if you have Parkinson’s and menopause? Why not! The breathing, the poses and the potential effects on menopause and on Parkinson’s make it an attractive choice.
In this blog will ask two experts to enlighten us on why yoga?
Who is Dr. Andrew McGonigle?
Dr. McGonigle attended medical school at The University of Newcastle Upon Tyne but struggled with the non-holistic approach often adopted by western medicine. He graduated in 2005 and worked for a brief period as a junior doctor in Sunderland Royal Infirmary. He started to practice Transcendental Meditation as a coping mechanism for stress and regularly attended hatha yoga classes and after a few years of dedicated practice, he decided to embark on an Ashtanga Yoga teacher training course at Yoga Thailand with Paul Dallaghan. He moved to London and worked at the triyoga headquarters where he remained in a Managerial role for almost 9 years. He began to set up his own small yoga classes in a local church hall and completed a holistic massage diploma with Quantum Metta in London. He was assisting on one of their massage courses when a student casually asked him why he wasn’t teaching anatomy. The thought had literally never crossed his mind - a true light bulb moment for him! He contributed several chapters to the Yoga Teaching Handbook: A Practical Guide for Yoga Teachers and Trainees and Yoga Student Handbook: Develop Your Knowledge of Yoga Principles and Practice. His new book, Supporting Yoga Students with Common Injuries and Conditions, was published in March 2021. His second book, The Physiology of Yoga, was published in June 2022. He teaches anatomy and physiology for the many Yoga Teacher Training courses and he has lead his own workshops and trainings across the UK and internationally. In 2020 he launched a Yoga Anatomy Online Course. Dr. McGonigle and Dr. Subramanian met at a yoga training and have shared many conversations about yoga and its potential benefits for people living with PD. Dr. Subramanian has a specific interest in women and PD and has been exploring ways to support through them through their hormonal transitions.
Dr. Andrew McGonigle is aka “ Dr. Yogi”- yoga teacher, anatomy teacher, medical doctor
This is an exclusive excerpt from his book, The Physiology of Yoga.
How to define menopause?
Menopause is defined as the permanent cessation of ovarian function and is thereby the end the reproductive phase (Sherman 2005). It is characterized by at least 12 months of amenorrhea (the absence of menstruation) (Gracia et al. 2005). Most people experience menopause between ages 40 and 58 (average age is 51) according to The North American Menopause Society. Physical changes begin years before the final menstrual period. This transition phase is called perimenopause and may last for 4 to 8 years. It begins with changes in the length of time between periods and ends 1 year after the final menstrual period. The perimenopausal time frame is not well studied in Parkinson’s disease, however it is a time when many women living with PD feel that their symptoms get worse. You can read more about women and PD in our blog.
How to cope with menopause
While it is an inevitable part of every woman’s life, about three out of every four people experience symptoms during menopause. Almost 90% of people seek out their healthcare provider for advice on how to cope (Guthrie et al 2003). These symptoms are often categorized into four subsets; psychological symptoms, for example, irritability, depressive feelings and mood swings; vasomotor symptoms, for example, numbness and tingling, hot flashes and lack of appetite; somatic symptoms, for example, gaining weight, headaches and insomnia; and urogenital, for example, loss of sexual interest and pain during intercourse. These symptoms often persist for several years after menopause (Cramer et al. 2012).
During the menopausal transition period, the drop of estrogen leads to more bone resorption than formation, which can lead to osteoporosis. Osteoporosis is a systemic skeletal condition characterized by low bone mass and micro-architectural deterioration of bone tissue which increases bone fragility and risk for fractures (U.S. Department of Health and Human Services 2004). The major health threat of osteoporosis is osteoporotic fractures. The prevalence of osteoporosis and related fractures increases in postmenopausal people (Ji and Yu 2015). Menopause is also a risk factor for cardiovascular disease; because estrogen withdrawal can have a detrimental effect on cardiovascular function and metabolism (Rosano et al. 2007).
Can Yoga Improve Menopause Symptoms?
Love this pic by Jonny Acheson as to whether hot yoga would be better?
There are conflicting reports from the published reviews and papers that have been conducted on the topic of whether yoga can improve the various symptoms of menopause. A systematic review by Lee and colleagues (2009) concluded that yoga was ineffective in relieving any menopausal symptoms including psychological symptoms. A systematic review and meta-analysis by Cramer and colleagues (2012) found moderate evidence for short-term effectiveness of yoga for psychological symptoms in menopausal people. However, no evidence was found for improvements regarding somatic, vasomotor, urogenital, or total menopausal symptoms. Further, no group difference was found when comparing yoga to exercise. A qualitative systematic review on mind–body interventions concluded that there was moderate evidence that yoga might relieve common menopausal symptoms including vasomotor and psychological symptoms (Innes, Selfe, and Vishnu 2010). The most recent systematic review and meta-analysis by Cramer, Peng, and Lauche (2018) reported that yoga seemed to be effective and safe for reducing psychological, somatic, vasomotor, and urogenital menopausal symptoms. These authors also noted that the effects were comparable to those of other exercise interventions. So, it appears that over the last decade, as the body of research on this topic has slowly grown, the benefits associated with practicing yoga for menopausal symptoms have become more evident.
Who is Petra Coveney?
Petra Coveney, founder of Menopause Yoga™, has been supporting people in menopause for over 10 years. As a member of the British Menopause Society for health practitioners, and a senior yoga teacher and trainer, she is committed to sharing information about the impact of hormone changes and of using yoga techniques that have been tried and tested in her workshops and classes. Petra says,
“When I’m teaching Menopause Yoga, I make it clear that yoga can never replace the hormones estrogen, progesterone and testosterone that all decline during the perimenopause to post menopause. So, any yoga teacher who claims to be able ‘rebalance your hormones’ is falsely selling snake oil to people, making claims that are not evidenced-based. People who are struggling with symptoms in the menopause transition can feel desperate and willing to try anything to improve their quality of life, so yoga teachers need to be careful not to over-sell or make false claims on the benefits of yoga.
What makes menopause yoga different than yoga?
“This is why Menopause Yoga is more than a series of yoga postures or breathing techniques; the context of the yoga practice is important too, and reframing it as a positive opportunity to improve our long-term health and wellbeing. People tell me they feel ‘scared, lost and alone,' and question if they are going ‘mad.’ So, Menopause Yoga includes circle discussions, so that we can break the taboo by talking about menopause and enjoy a sense of community.”
“As you know, these hormones are not just for fertility; they support the whole body, including brain, bones and heart health. So, I encourage people to include yoga as part of a holistic self-care approach that may include HRT, nutrition, herbal remedies, complimentary and talking therapies depending on the person's needs.”
What specific types of yoga should I do with menopause?
“Although research shows that yoga can be as beneficial as other forms of exercise in managing menopause symptoms, what I found when researching my book Menopause Yoga, was that there was little information about what specific types of yoga, meditation or breath-work were used in the research studies (many authors simply say Hatha yoga). Simply saying yoga may or may not help with menopause symptoms; is too simplistic and reveals the researchers’ lack of insight into the different styles and practices. For instance, the faster-paced Ashtanga yoga practice may not be helpful for people experiencing anxiety or muscle and joint pain; however a somatic slow flowing practice leading to restorative yoga may help. Hot yoga will increase physical heat for people having hot flashes, but they may benefit from cooling and calming pranayama techniques. Restorative yoga can help people with fatigue and reduce stress levels, which can alleviate the sensation of some symptoms and benefits their general health. To build bone density, muscle strength, and heart health, we need to practice longer held yoga poses that stack the joints, lift the heart rate and challenge your balance. “
So in summary, if you have Parkinson’s and menopause, yoga could be a great option.
Selected References:
Cramer, H., R. Lauche, J. Langhorst, and G. Dobos. 2012. “Effectiveness of Yoga for Menopausal Symptoms: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Evidence-Based Complementary and Alternative Medicine 2012: 863905.
Cramer, H., W. Peng, and R. Lauche. 2018. “Yoga for Menopausal Symptoms—A Systematic Review and Meta-Analysis.” Maturitas 109:13-25.
Gracia, C., M. Sammel, E. Freeman, H. Lin, E. Langan, S. Kapoor, and D. Nelson. 2005. “Defining Menopause Status: Creation of a New Definition to Identify the Early Changes of the Menopausal Transition.” Menopause 12 (2): 128-135.
Guthrie, J., Dennerstein, L., Taffe, J., and Donnelly, V. 2003. “Healthcare-seeking for menopausal problems.” Climacteric 6: 112–117.
Innes, K., T. Selfe, and A. Vishnu. 2010. “Mind–Body Therapies for Menopausal Symptoms: A Systematic Review.” Maturitas 66 (2): 135-149.
Ji, M., and Q. Yu. 2015. “Primary Osteoporosis in Postmenopausal Women.” Chronic Diseases and Translational Medicine 1 (1): 9-13.
Lee, M., J. Kim, J. Ha, K. Boddy, and E. Ernst. 2009. “Yoga for Menopausal Symptoms: A Systematic Review.” Menopause 16 (3): 602-608.
Rosano, G., C. Vitale, G. Marazzi, and M. Volterrani. 2007. “Menopause and Cardiovascular Disease: The Evidence.” Climacteric 10 (Suppl. 1): 19-24.
Sherman, S. 2005. “Defining the Menopausal Transition.” American Journal of Medicine 118 (Suppl. 12): 3-7.
U.S. Department of Health and Human Services. 2004. Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville, MD: DHHS.