What did the experts who met in Sweden this week say we should focus on with Parkinson's?
I (Dr. Subramanian) attended my first live meeting since the COVID pandemic hit. I have been reflecting on my biggest take-aways from this “awesome” meeting. The group of clinicians and scientists who focus on non-motor issues are amazingly collaborative and are really are focused on what matters to people living with PD. The meeting was beautifully arranged by Prof Chaudhuri and Prof Per Odin from Lund University and was generously locally hosted by Ulrika Mundg-Petersen. It was organized by the Non-motor study group of the Movement disorders society. It was my great honor and privilege to attend and I profusely thank the organizers for including me.
1. The continued importance of non-motor issues in
Quality Of Life in Parkinson’s.
The field of “non-motor issues in PD” has been championed by Prof K Ray Chaudhuri from King’s College, London, England and by many other international investigators. Ray has spent the last 2+ decades helping clinicians to recognize the importance of symptoms such as pain, fatigue and cognition. In this recent meeting, speakers highlighted issues such as: non-motor symptoms (NMS) during early and late stages of PD; the speakers also commented on the importance of non-motor issues in the time of covid.
2. Emergent need to address Racial Disparities in
Parkinson’s.
Every corner of the planet has issues with unmet needs in medical care— and COVID has highlighted many pressing issues. Populations at risk frequently mistrust the scientific groups— we must together think of ways to change this scenario, from the ground up. Training more clinicians in these unmet populations could be critical— for example if we train more Black movement disorders fellows in the USA and the UK it may place us in a position to better dialogue with these communities. We need to be delivering education and care (not just including minority populations in studies). We need to open our minds to what we are doing and what we have done wrong in the past. We must be reflective of the reality that we have done a poor job in including minorities into research studies. Prof Anette Schrag and Dr. Alastair Noyce are some of the researchers working on this problem (they are located in the UK). By learning more about PD and how it effects different populations, the hope is that we can address issues for all PWP (we need a more diverse strategy).
3. Gender disparities are another huge unmet
need in Parkinson’s.
Gender disparities came up over and over at the meeting. It is amazing how many unmet needs there are in this area including in Deep Brain Stimulation Surgery. Many women do not want surgery— even when offered it. It has been unclear what the barriers are for women to get DBS, since following surgery, many women report superior DBS outcomes than men. There are also important gender-specific caregiver issues and non-motor symptoms that have begun to draw the attention of the experts. We will likely require better ways to address “mistrust in the community.” We need to understand why patients don’t receive or even want certain types of care. Improving communication, addressing engagement, providing access and paying attention to the required support for women living with PD— these should be priorities for 2021 and beyond. Prof Moro beautifully highlighted many of these issues during the meeting. The Women’s Parkinson’s Project has is a great place to seek information on this topic.
4. Other issues in the body can effect Parkinson’s
and guess what? Parkinson’s can affect other “body”
issues.
The speakers at the meeting pointed out that areas such as vision, bone health, and dental care are important and there can be profound effects on symptoms of PD. PD is truly a multi-disciplinary endeavor- and though we sometimes forget, the speakers highlighted the importance of dentists, speech therapists and primary care docs. Ask yourself whether addressing some of the not Parkinson’s problems could benefit the Parkinson’s treatment or overall treatment outlook.
5. Mental health issues are major and we are not
doing a good job with them.
Anxiety and depression are very common, and have been especially troublesome and amplified during the pandemic. We need to find ways to care for and to study these phenomena remotely. We need (as a field) to engage and to collaborate with more mental health specialists. We need to train other providers to identify and triage mental health issues in our vulnerable population and to make sure appropriate referrals are made. Dr. Weintraub from the Philadelphia VA is a world leader in mental health care and a great resource.
6. Loneliness/social isolation have profound effects
on caregivers (who can be) located all over the
planet.
Loneliness was a universal theme throughout the meeting and one that has been understudied. I (Dr. Subramanian) presented my data on loneliness and Parkinson. I believe we need need to engage and to train other types of intermediary providers in an effort to best support our patients. We need to be proactive and to screen patients, engage in online support and to help patients find buddies or mentors in the community.
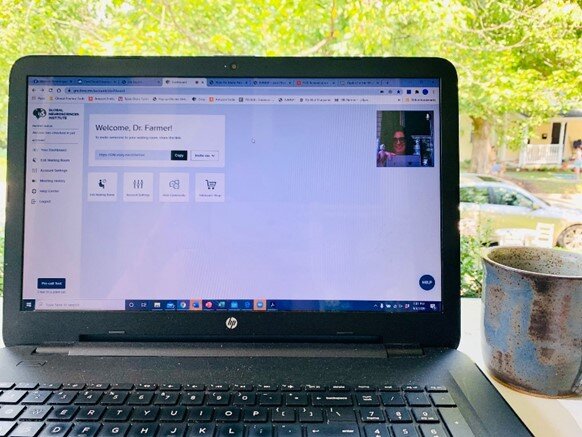
7. Telehealth is and will be the way of the future.
We critically need to discover better ways to reach populations and to validate the screening tools we use. Using online platforms (for example for cognition screens) may be critical. The future will likely include more apps and more remote monitoring.
8. Wellness and lifestyle strategies are of interest in
many populations and not just for Parkinson’s.
There is a condition called prodromal PD if we identify populations at risk of getting PD what would we tell them to do?). How about how passing a positive message of support for patients sheltering in place and possibly patients who have had covid and may be at risk for long- covid complications. Long covid could affect cognition, mood , fatigue, apathy and other symptoms. The speakers discussed the importance of sleep, diet, exercise and mind-body approaches (such as yoga, mindfulness and social connection). There are so many options and we need to be more open-minded. The expert group was very open minded to this new area of studying wellness and lifestyle in Parkinson’s disease.
9. How much have I missed human connection in a
“real” live in person meeting.
More than you can imagine! I know if “in-person” is important for me, it must be important for everyone with Parkinson’s too.
To read more books and articles by Michael S. Okun MD check on Twitter @MichaelOkun and these websites with blogs and information on his books and http://parkinsonsecrets.com/ #Livingwith Parkinson’s #EndingPD #Parkinsonsecrets #LessonsFromTheBedside
He also serves as the Medical Advisor for the Parkinson’s Foundation.
To see more on Dr. Indu Subramanian she does live interviews of experts in Parkinson’s for the PMD Alliance.
The blog artist is Jonny Acheson.