The 5 Myths of Swallow Dysfunction in Parkinson Disease and the Tips to Fix Swallowing
Who is Nicole Herndon?
Nicole Herndon is a speech-language pathologist at the University of Florida Health Rehabilitation Center at the Norman Fixel Institute for Neurological Diseases in Gainesville, Florida. She earned her Bachelor and Master of Science degrees in Speech-Language Pathology in 2014 from Purdue University. She received her Certificate of Clinical Competence (CCC-SLP) in 2015 while working at a private practice in Fairfax, Virginia. In April 2018, she joined the multidisciplinary team at the Norman Fixel Institute where she provides speech, swallowing, and/or cognitive-linguistic evaluations as well as treatments. She has presented at local and national conferences regarding speech and swallowing in Parkinson’s disease, parkinsonism, and effects of deep brain stimulation. In addition, she is a courtesy faculty for the University of Florida’s Department of Speech, Language, and Hearing Sciences. She is a member of the American Speech-Language-Hearing Association (ASHA).
We sat down with Nicole and we picked her brain about myths and tips for swallowing in Parkinson’s disease. To watch the PMDalliance session with Dr. Subramanian and Nicole Herndon please watch
What does a speech language pathologist do?
Swallowing occurs around 1,000 times per day and takes a matter of seconds to complete. There are approximately 50 pairs of muscles activated with each swallow. But what happens if there is a breakdown in the act of swallowing?
Dysphagia is defined as difficulty swallowing or “problems involving the oral cavity, pharynx, esophagus, or gastroesophageal junction” by the American Speech-Language-Hearing Association (ASHA; www.asha.org). As speech-language pathologists, we evaluate and treat swallowing dysfunction that occurs in the mouth or throat, which we call oro-pharyngeal dysphagia.
By; JOnny Acheson
Myth #1 – Parkinson’s disease does not impact swallowing.
Up to 80% of individuals with Parkinson’s disease will have swallowing changes that occur over the course of their disease. Swallowing changes occur across all 3 stages of swallowing: oral, pharyngeal, and esophageal (Figure 1). The severity of these changes can range from minor changes without any functional impact to severe changes impacting quality of life. Research has shown that the longer the disease duration, the more likely there will be dysphagia. However, research has also shown that swallowing changes and variability can occur in the early stages of many diseases (e.g. Parkinson’s disease). Why is swallowing impacted in Parkinson’s disease? It is not clear at this time. It is thought that rigidity (stiffness) and bradykinesia (slowness of movement), which are 2 of the 4 hallmark signs of Parkinson’s disease, can also impact muscles in all 3 stages of swallowing.
Myth #2 – I would know if I had swallowing changes.
Actually, no. It depends on what swallowing changes have occurred. Symptoms of dysphagia are often under-reported or unidentified as compared to results observed with more in-depth instrumental swallowing evaluations (modified barium swallow study (MBSS) or a flexible endoscopic evaluation of swallowing (FEES).
Drooling: The sensation of excess saliva and drooling can be noticeable. For some, this occurs only when distracted or bending over to pick something up off the ground, whereas for others, this occurs throughout the day. Drooling occurs due to reduced spontaneous swallowing frequency, thus resulting in saliva accumulation in the mouth. Treatments may include swallowing more frequently, sips of water, sugarless gum/candies or lozenges, medication, or botulinum toxin injections directly to the salivary glands.
Dry mouth: This can be a side effect of the medications taken for Parkinson’s disease or due to breathing through the mouth (versus nose, which provides humidification). Treatments may include more frequent sips of water, products marketed for dry mouth such as Biotene or ACT, sugarless gum/candies/lozenges, or synthetic saliva. Also, for oral care, make sure to use alcohol-free mouthwash soas to not cause more dryness —like with alcohol-based produced.
Aspiration: First off, it is important to note that we all aspirate (we breathe food and particles into the lungs)! However, we are concerned about the frequency, amount, and contents (i.e. bacteria) of material aspirated. Aspiration occurs during the pharyngeal phase of the swallow and is defined as “entry of secretions, food, or any foreign material into the airway that travels below the level of the vocal folds” by ASHA (www.asha.org). It can also occur from reflux of stomach contents.
Cough: When one aspirates, the body attempts to eject the aspirated material with coughing or throat clearing. In those with Parkinson’s disease, a diminished or absent cough response to aspirated material has been shown. Therefore, you cannot rely on the absence of coughing during meals as an indication of normal swallowing function.
Choking: Choking may require the Heimlich maneuver. It may or may not be due to underlying swallow dysfunction.
Residue: Sticking of material in the mouth, throat, or esophagus may occur. One’s ability to precisely locate residue in the throat or esophagus is not always accurate despite sensing it in a specific location.
Mouth: it may take longer to move the food, pills, or liquid into your throat or to initiate a swallow. For some, placing pills further back on your tongue or putting pills in a puree/pudding consistency may be helpful.
Throat: There are multiple reasons this may occur such as reduced squeezing of the muscles to move the material into the esophagus.
Esophagus: If food or pills stick in the esophagus or reflux occurs, a gastroenterologist may be needed to complete an assessment to evaluate the esophageal stage of swallowing.
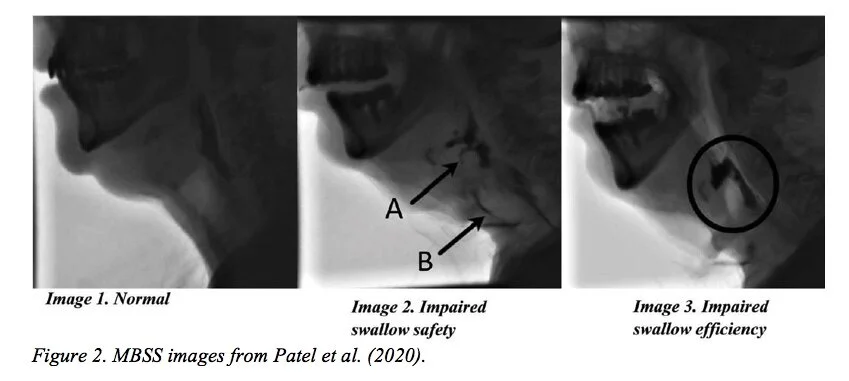
Breathing Coordination for Swallowing: Coordination of breathing and swallowing can be impacted in individuals with Parkinson’s disease. Typically, after you swallow, you exhale. Try it! This may not always be the case for those with Parkinson’s disease. Instead, they may inhale after a swallow, which may place them at a higher risk for aspiration of residue. The best way to identify oro-pharyngeal swallowing changes is by undergoing an instrumental evaluation with a modified barium swallow study (MBSS) (Image 1) or with a flexible endoscopic evaluation of swallowing (FEES). Talk with your neurologist about an instrumental evaluation to assess your oro-pharyngeal swallow if you are having symptoms or are interested in a baseline swallowing evaluation.
Myth #3 – We only care about aspiration.
When your neurologist or speech-language pathologist requests an instrumental evaluation to assess your oro-pharyngeal swallow function, it is so we can check the safety and efficiency of swallow as well as to try strategies, diet modifications, and identify targets for therapy (if warranted).
• Sometimes thicker liquid is not safer or more efficient.
• Avoiding straws or tucking your chin do not always improve swallow function. In fact, they could worsen one’s swallow function in certain cases.
Safety includes making sure you protect your airway effectively soas to not experience aspiration (Figure 2: Image 2). Efficiency includes making sure you can efficiently move material from the mouth into the esophagus soas to not have residue (Figure 2: Image 3).
We will not know what helps the individual with Parkinson’s disease until we see it during an instrumental evaluation. If you are experiencing swallow difficulties or are concerned about swallow changes with your Parkinson’s disease diagnosis, talk with your neurologist about ordering an instrumental evaluation to evaluate the safety and efficiency of your oro-pharyngeal swallow.
Myth #4 – Aspiration alone leads to aspiration
pneumonia.
It’s a complex process. Other factors are involved as well. Aspiration is when a substance such as food, liquid, reflux, bacteria, or a virus enters the lungs. Factors that influence the development of aspiration pneumonia include poor oral hygiene, being immunocompromised, use of numerous medications such as sedatives, and reduced respiratory/lung function. Aspiration pneumonia is considered the leading cause of death in individuals with Parkinson’s disease. How can you reduce your risk of developing aspiration pneumonia? A simple way is with good oral care.
• Oral care reduces bacteria in your mouth.
• This includes brushing your teeth, tongue, and gums at least 2 times per day. Friction from brushing is important to reduce bacteria on the oral surfaces.
• If you have dentures or a limited number of teeth, you still need to complete oral care at least 2 times per day as bacteria continues to grow in the mouth.
• Regular dental cleanings at least every 6 months is also recommended.
Myth #5—There is nothing that can be done to improve my swallow.
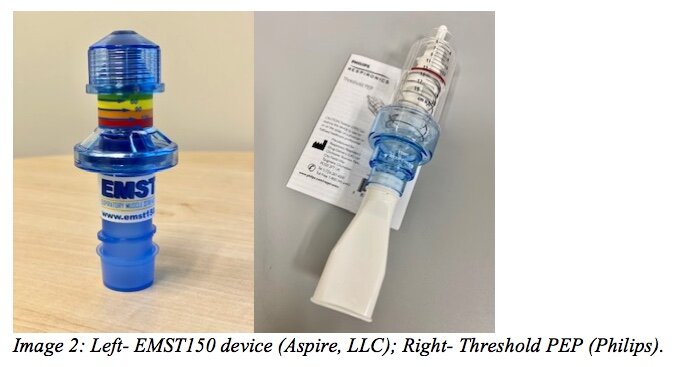
Maybe…it depends on the swallowing problems identified and reasons for those issues. Simply speaking, just like you can strengthen your arms and legs with exercise, you can strengthen the swallowing muscles. Troche and colleagues (2010) study found the use of expiratory muscle strength training (EMST) to treat reduced swallow safety in those with Parkinson’s disease was helpful. This involves exhaling into an adjustable pressure threshold device (image 2) with enough pressure to successfully open the valve. The device should be set-up with the help of your speech-language pathologist to make sure it is set to the correct level.
There is also some evidence supporting the use of speech exercise programs such as Lee Silverman Voice Treatment – LOUD (LSVT LOUD; www.lsvtglobal.com) and SPEAK OUT! (www.parkinsonvoiceproject.org) to improve swallow function. Additionally, there are other swallowing exercises that can be prescribed by your speech-language pathologist.
Final Tips for Swallowing
Overall, swallowing changes or dysphagia are known to occur in Parkinson’s disease regardless of disease duration.
General Swallowing Strategies:
• Limit distractions during meals.
• Do not talk with food or liquid in your mouth.
• Always eat and drink in an upright position.
• Oral care, oral care, oral care! At least 2 times per day and please always seek routine dental appointments.
An instrumental evaluation (MBSS/VFSS or FEES) will be needed to:
1. Specify swallowing changes that have occurred,
2. Provide recommendations for appropriate strategies and diet,
3. Identify information for individualized swallow therapy exercises. Please discuss any swallowing difficulties or symptoms with your neurologist and speech-language pathologist.
Parkinson’s Swallowing Resources:
American Speech-Language-Hearing Association: www.asha.org/Practice-Portal/Clinical-Topics/Adult-Dysphagia/
Parkinson’s Foundation: https://www.parkinson.org/pd-library/books/speech-swallowing
The Michael J. Fox Foundation: https://www.michaeljfox.org/news/speech-swallowing-problems
This blog is brought to you by Michael S. Okun and Indu Subramanian.
To read more books and articles by Michael S. Okun MD check Twitter @MichaelOkun and these websites with blogs and information on his books and http://parkinsonsecrets.com/ #EndingPD #ParkinsonPACT #Parkinsonsecrets and https://www.tourettetreatment.com/
He also serves as the Medical Director for the Parkinson’s Foundation.
To see more on Dr. Indu Subramanian she does live interviews of experts in Parkinson’s for the PMD Alliance
References:
Curtis, JA, Molfenter, SM, & Troche, MS. (2020). Pharyngeal area changes in Parkinson’s disease and its effect on swallowing safety, efficiency, and kinematics. Dysphagia, 35(2), 389-398.
Miles, A., Jardine, M., Johnston, F., de Lisle, M., Friary, P., & Allen, J. (2017). Effect of Lee Silverman Voice Treatment (LSVT LOUD®) on swallowing and cough in Parkinson’s disease: A pilot study. J Neurol Sci, 2017 Dec 15; 383: 180-187.
Patel, B., Legacy, J., Hegland, K.W., Okun, M.S. & Herndon, N.E. (2020). A comprehensive review of the diagnosis and treatment of Parkinson’s disease dysphagia and aspiration, Expert Review of Gastroenterology & Hepatology, 14:6, 411-424, DOI: 10.1080/17474124.2020.1769475
Suttrup, I. & Warnecke, T. (2016). Dysphagia in Parkinson’s disease. Dysphagia, 31, 24–32.
Troche, MS, Schumann, B, Brandimore, AE, Okun, MS, & Hegland, KW. (2016). Reflex cough and disease duration as predictors of swallowing dysfunction in Parkinson’s disease. Dysphagia, 31(6), 757-764.
Troche MS, Okun MS, Rosenbek JC, Musson N, Fernandez HH, Rodriguez R, et al. Aspiration and swallowing in Parkinson disease and rehabilitation with EMST: A randomized trial. Neurology. 2010 Nov 23;75(21):1912–9. .