How to 'integrate' integrative medicine for Parkinson's disease?
By Indu Subramanian MD
Can we focus on the person with Parkinson’s disease and still be informed by the evidence? You bet we can. Can we achieve optimal health and healing by focusing on what matters most? Yes we can. Can we shift the person with Parkinson’s from a state of pure survival, to one of thriving? It is possible. In this months blog, I will, with help from Dr. Sushma Kola from Northwestern University, teach you about integrative medicine and share tips on how to ‘integrate’ them into your overall Parkinson’s strategy.
Check out our newest paper on Integrative Medicine in Parkinson’s which was published on November 3, 2023.
Brian Grant, former NBA player and person with Parkinson’s along with Dr. Indu Subramanian. Together they are getting their ‘integrative medicine’ groove on. The other two pictures are LEGO teaching images from our parkinsonsecrets.com artist Jonny Acheson, who is also a person with Parkinson’s.
What is integrative medicine?
The Consortium of Academic Health Centers for Integrative Medicine defines integrative medicine as “the practice of medicine that reaffirms the importance of the relationship between practitioner and patient (person with disease), focuses on the whole person, is informed by evidence, and makes use of all appropriate therapeutic approaches, healthcare professionals, and disciplines to achieve optimal health and healing.”
This concept aligns with the World Health Organization (WHO) definition of health:
“a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity”.
How should we be shifting Parkinson’s disease into an integrative approach?
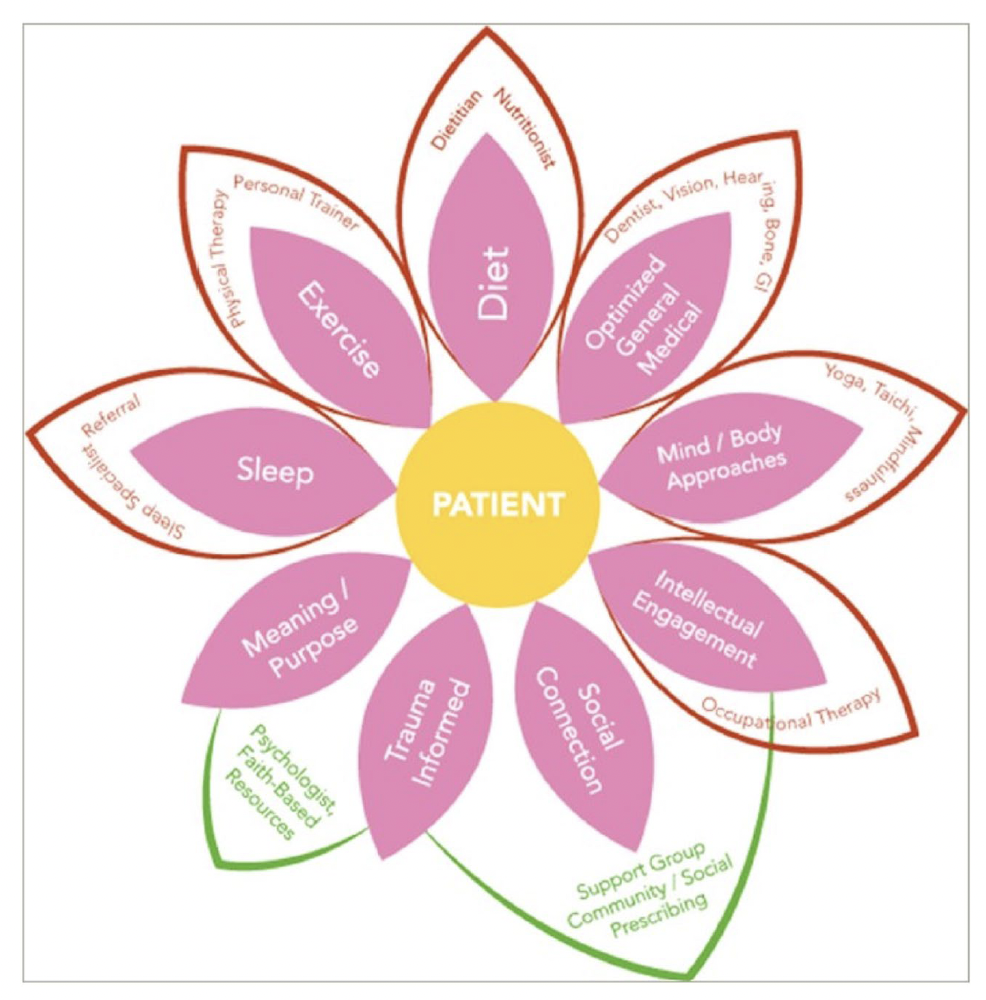
Great paper by Drs Subramanian and Kola in Current Neurology and Neuroscience Reports 2023. This figure encapsulates the many aspects to integrative care in Parkinson’s disease.
Shifting the Parkinson’s disease treatment paradigm into an integrative approach should:
Place the person with disease at the center of the care team.
Give the person with disease the agency to clearly define their care goals.
PD management should be tailored to what matters most physically, mentally, spiritually, and culturally.
By considering these three areas the person with disease can be empowered to gain control over their daily lifestyle choices. These choices can influence health outcomes.
In a Parkinson’s disease integrative medicine approach instead of surviving, we can work to shift the person into a state of ‘thriving.’
What are the most important components of integrative medicine?
For a person with Parkinson’s disease, the most important components of integrative medicine are physical activity, nutrition, sleep, social connection, and mind–body therapy(s).
An integrated treatment approach proactively targets these components to improve both Parkinson’s disease motor and non-motor symptoms, independence, resilience, well-being and also quality of life.
A very interesting study of complementary medicine approachesappeared here: https://thehealingclinic.org/integrative-medicine-the-next-big-idea-in-holistic-health/ This gives us the sense of what people are actually doing in the community; and it also emphasizes that strategy is needed to move true integrative medicine to the next level.
Are there evidence-based integrative medicine treatments?
There are evidence-based treatments which can be applied to integrative medicine approaches. We offer some practical tips on physical activity, nutrition, sleep, social connection and mind-body practices in the table below.
Kola S, Subramanian I. Updates in Parkinson's Disease Integrative Therapies: an Evidence-Based Review. Curr Neurol Neurosci Rep. 2023 Nov 3. doi: 10.1007/s11910-023-01312-z. Epub ahead of print. PMID: 37921943.
How should I think about exercise as an integrative medicine approach?
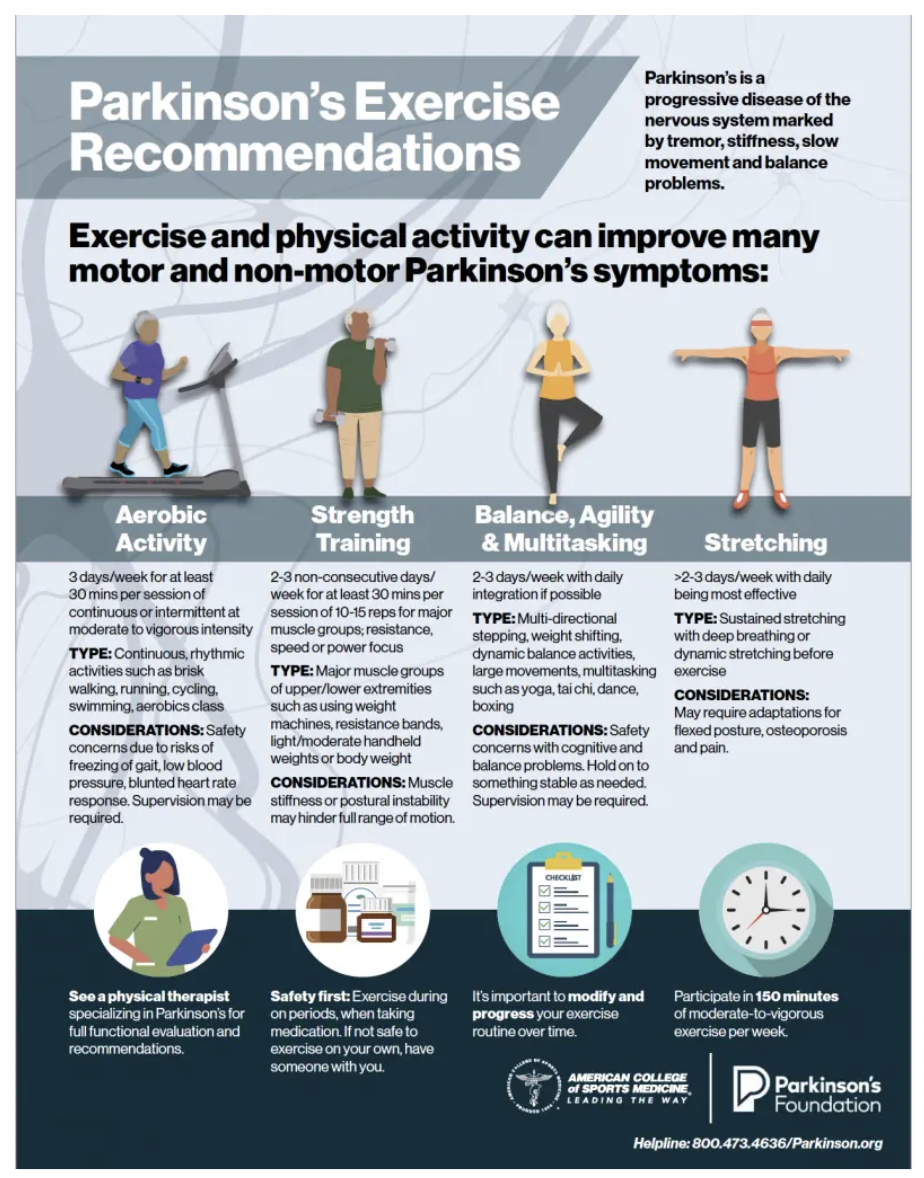
The Parkinson’s Foundation recommends ~150 min per week of moderate to vigorous intensity exercise.
A well-rounded exercise regimen should include aerobic activity, strength training, balance drills, and stretching.
Exercise in Parkinson’s disease is a heavily researched area and there are many positive randomized controlled trials.
Exercise is a key component of almost all integrative medicine approaches and we love this wheel of health from Duke Medicine.
Aerobic Exercise
Aerobic exercise has been found to alter brain structure and function. For the geeks, these brain areas would include increasing caudate nucleus dopamine release, activating the ventral striatum and enhancing functional connectivity of the putamen.
Exercise may reduce global atrophy (brain size), may improving cognition and in some cases stabilize disease progression.
High-intensity lower extremity aerobic exercise has been shown to improve bimanual coordination of grasping. This type of movement is important for activities of daily living.
Exercisers improve sleep efficiency and quality.
A gamified home-based, remotely supervised aerobic exercise program improved motor scores in one recent study at 6 months. What is cool about this finding is that the therapy could be moved into the home setting.
Walking for exercise has been investigated extensively. Studies vary in recommending 4200 steps daily to ~7500 steps. In one study, a community-based brisk walking program was superior to upper limb training in alleviating motor symptoms and in promoting balance and gait performance.
Cycling is another popular aerobic training modality and evidence in amassing; a large multi-center study getting underway. Cycling safely in Parkinson’s may possibly be accomplished by in home recumbent exercise bikes.
Strength and Resistance Training
Core exercises have been a recent focus of strength training in Parkinson’s disease. Core stabilization, pilates and trunk-specific strength training programs may improve postural stability and balance.
Resistance training requires pushing or pulling against the resistance of an object. It may be more effective than conventional motor rehabilitation in improving freezing of gait, motor function, anxiety, quality of life and possibly brain plasticity.
Most experts recommend prescribing a balanced exercise routine and strategies to increase compliance for every person with Parkinson’s disease.
Rehabilitation
Persons with Parkinson’s disease will likely benefit from working with specialized physical, occupational and speech therapists for evaluations of function and for personalized exercise recommendations. Even better is when each of the specialists effectively communicate (multidisciplinary care).
The Lee Silverman Voice Treatment-BIG (LSVT-BIG) program is one example program which may have benefits beyond voice therapy. There are many other examples and seeing a physical therapist, occupational therapist or speech therapist who is familiar with the guidelines for best practices in Parkinson’s disease can be very helpful. Many organizations and societies have published guidelines, and if your therapist is not available with them it could be helpful for you to print them and bring them to your appointment.
One example of information and guidelines can be found on the Parkinson’s Foundation website.
Virtual reality programs for rehabilitation are now possible and may offer the advantage of improved access.
Many foundations like the Parkinson’s Foundation have a lot of information in recent guidelines for use of rehabilitative therapies and exercise.
What is the bottom line for integrating exercise and specialized therapy recommendations in Parkinson’s disease?
A balanced exercise routine should include ≥ 150 min/week of moderate-intensity aerobic exercise and ≥ 2 days/wk of strength and balance training and finally access to comprehensive rehabilitation specialists and interventions.
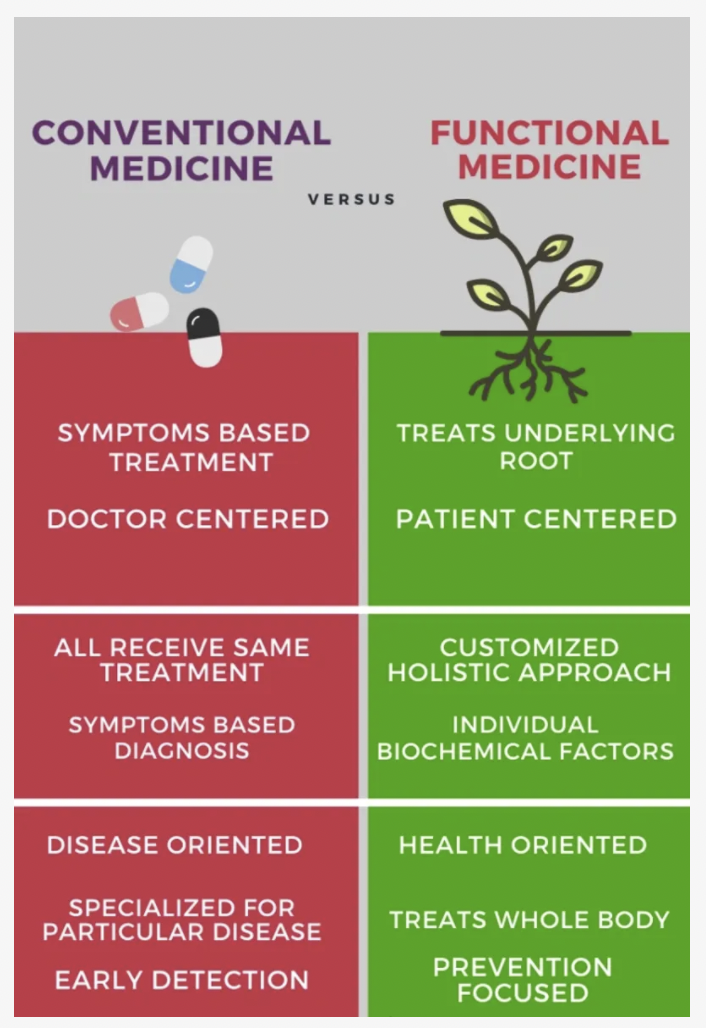
Do you know the difference between conventional and functional medicine. We found this chart here: https://dawsonmedicalcenter.com/functional-medicine which was a succinct comparison.
What about integrating diet and nutrition?
There is no officially established Parkinson’s diet, although adherence to the Mediterranean diet has been associated (in a few small studies) with a lower risk of developing prodromal and symptomatic PD as possibly a slower disease progression in those who may already have disease.
The Mediterranean diet emphasizes plant-based foods (fruits, vegetables, whole grains) and moderate amounts of fish and dairy, with olive oil as the main source of healthy fat. Little to no red meats or sweets are consumed in this diet.
In a recent randomized controlled trial, the Mediterranean diet was found to improve the cognitive domains of executive function, attention, concentration, language, and active memory. In this single small study, the diet increased serum total antioxidant capacity and decreased the UPDRS motor Parkinson score.
A trial is currently underway to determine whether a Mediterranean diet can improve gastrointestinal function and constipation.
In a recent small study comparing a low fat high carbohydrate diet with a ketogenic diet, both groups had improved motor and non-motor symptoms .
A recent review examining the impacts of a healthy diet, a Mediterranean diet, the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet, a protein-restricted diet and of a ketogenic diet overall the verdict was inconsistent results. It is therefore hard to be absolute about choosing diet in Parkinson’s disease.
The bottom line is that eating healthy and integrating a consistent diet into your Parkinson’s strategy will likely pay dividends. Choose the diet that you will be compliant with and the one you feel the best when taking it. Most of the current evidence supports the Mediterranean diet. Remember that giving your medications ‘1/2-1 hour head start’ before you eat will promote better absorption.
What diet will you choose after shared decision making?
https://www.forksoverknives.com/wellness/do-people-need-different-diets/
Probiotics
Gastrointestinal dysfunction commonly manifests as constipation, nausea, and bloating in Parkinson’s disease.
Constipation affects up to 90% of persons with Parkinson’s and it may precede the onset of motor symptoms in some cases.
What about using probiotics for constipation and for the motor and non-motor Parkinson’s symptoms? There is some data suggesting that a multi-strain probiotic containing lactobacillus and bifidobacterium improved gut transit time and also improved bowel movement frequency. There may be benefits in constipation symptoms, stool consistency and quality of life. Some early studies have even suggested that probiotics may improve motor function, mood, cognition and sleep.
At present however, no specific recommendations can be made regarding specific strains or quantities of probiotics. In fact, the microbiome is changed when you take a probiotic, so it is possible that it may also in some cases worsen absorption of your medications and possibly even worsen your symptoms.
Though most experts do not routinely recommend probiotics, they are relatively safe. Because of the lack of data, shared decision making is recommended and a monitoring program should be implemented to determine if ‘the juice is worth the squeeze.’
When it comes to integrating diet into our recommendation, we current favoring a balanced diet prioritizing fruits, vegetables and whole grains and limiting processed foods, red meats, and sweets. We should mention that more research needs to be done in diet and Parkinson’s disease; it is not a one size fits all.
What about integrating better sleep?
Sleeping tips for Parkinson’s Europe.
Sleep disturbances are pervasive in Parkinson’s disease and there are actually many different types. Sleep dysfunction can be a major source of disability, and has a high likelihood of impairing quality of life.
Some studies have suggested that insomnia and sleep walking may be independent risk factors for developing Parkinson’s disease.
Restorative sleep is crucial, and it is imperative that healthcare professionals promote appropriate strategies to promote excellent sleep.
Studies have suggested that your circadian rhythm is bi-directionally impacted by healthy behaviors, including exercise and diet.
In persons with Parkinson’s, treatment of sleep disorders such as obstructive sleep apnea, REM sleep behavioral disorder and insomnia may improve cognition, attention and depression.
Bright light therapy has been associated in some studies with better sleep quality, but so far there is not a lot of evidence showing depression, anxiety or fatigue improved.
We recommend optimal sleep health for everyone with Parkinson’s. Optimal sleep health is characterized by sufficient duration, efficiency, regularity, alertness, timing and sleep satisfaction.
Your ‘sleep routine’ should be reviewed by your doctor and team and proactively leveraged to improve health and well-being.
A great nights sleep is the key to a great next day!
Finally, if you are sleepy or fatigued during the day, consider seeking screening for a sleep disorder.
The ‘Epworth Sleepiness Scale’ is one tool which can quickly assess for daytime sleepiness. The Epworth is a series of questions; taking this quiz may help to determine whether you will need a formal sleep study. This tool ranks the risk of ‘dozing off’ during various activities such as reading, watching TV, sitting and even driving.
What about integrating social engagement?
Nice piece by Alzheimer’s Disease New Jersey emphasizing how important social engagement is to neurodegenerative diseases.
Persons with Parkinson’s are more susceptible to social isolation and loneliness. This may be due to older age, the stigma of chronic illness and possibly due to embarrassing or distracting symptoms. This can add up to social withdrawal.
An increasing body of literature has demonstrated that loneliness has led to worsening of Parkinson’s non-motor features including depression, anxiety, apathy, cognition, fatigue and sleep. Ultimately, loneliness has been associated with worsened Parkinson’s disease severity and quality of life .
A survey of patients and caregivers identified a major culprit to be the decline in physical engagement and social support from outside the household.
One intervention to boost well-being and to reduce loneliness may be social prescribing or referring persons for social support.
It is crucial that this prescribed support addresses the three spheres of social interaction: intimate/emotional, relational/social, and collective interactions.
The first sphere can be achieved with the intimate connection of a marriage or partnership, while the second sphere relates more to social engagement with close friends. Finally, the third sphere can be achieved by belonging to a group with a shared sense of purpose; a Parkinson’s support group, a book club, a group exercise class or a religious group.
Newsflash: Happily married people can still be lonely especially if they lack a circle of friends or a community with a shared sense of identity. Therefore, an optimal social prescription incorporates all three spheres of loneliness, emphasizes quality of contact over quantity and is employed in combination with exercise, healthy diet and of course refreshing sleep.
Cognitive behavioral therapy (CBT) is an intervention with strong evidence in combating loneliness. Cognitive restructuring allows people to reframe feelings of loneliness, regain self-agency and to target perceptual biases that make them prone to isolation.
CBT for loneliness can be accessed in-person (individual and group sessions) or virtually. Telehealth mindfulness-based CBT for depression and anxiety had mixed results in randomized controlled trials, but did improve quality of life. We have a lot to learn about how to use CBT in Parkinson’s disease.
To screen for loneliness, we suggest to ask yourself "Do you sometimes feel left out?" and "Do you sometimes feel isolated from others?"
Finally, consider the cultural context when designing an intervention for lonliness.
Have you considered more than your traditional systems of medicine?
Ayurveda
Ayurveda is an officially recognized system of medicine that originated in South Asia and is thousands of years old. It focuses on the principle that optimal health exists when the body, mind and soul are balanced.
Diseased and healthy states are determined by the interplay of three doshas, or constitutions: vata (air and ether), pitta (fire and water), and kapha (water and earth). Vata is described as the energy of action, transportation, and movement. Pita represents the energy of transformation, conversion, and digestion. Kapha is the energy of construction, lubrication, and nourishment.
One interesting feature about this form of medicine is that it considers body build, speech pattern, digestion, temperature preference, bowel habits and emotional tendencies to determine one’s active dosha(s). When these are unbalanced, dietary and lifestyle changes may help to restore harmony and to promote healing.
Formal training in Ayurvedic medicine consists of 5 to 8 years of study in South Asia or 1 to 3 years of study in the United States.
Ayurvedic traditions including yoga and meditation can be used in combination with conventional treatments and some have now been studied in randomized controlled trials. For example, some studies suggest that when compared to stretching and resistance exercises, mindfulness yoga was superior in improving depression, anxiety, spiritual well-being and quality of life. Mindfulness yoga was equally effective in ameliorating mobility and motor dysfunction. Results of these limited studies do however, need to be interpreted with caution. Another example in the literature was Hatha yoga improving mobility, balance, gait and fall frequency. Finally, some studies have suggested that Yoga and walking meditations enhance balance and reduce disease severity.
Nice picture of mucuna pruriens the legume with dopamine from the American Parkinson’s Disease Association.
Mucuna pruriens is a levodopa-containing tropical legume, that has been used for centuries in traditional Ayurvedic medicine. When combined with a decarboxylase inhibitor, Mucuna was found to be non-inferior to synthetic carbidopa/levodopa in motor efficacy and safety, while also providing the potential for better ON dopaminergic time (and fewer dyskinesias). These results should be interpreted with caution as the study was very small. Wide prescribing of mucuna may not be a good idea because of the lack of clear dosing guidelines and different preparations. Mucuna may be a treatment of choice in parts of the world where levodopa is not yet available tand may offer 3rd world economies a more affordable option to make levodopa available to the masses. Finally be careful of mucuna ordered off the internet as purity and composition are unknown and not regulated.
Traditional Chinese Medicine
Nice picture of Tai Chi and Parkinson’s disease from Parkinson’s UK.
Traditional Chinese medicine (TCM) is a 2000-year-old East Asian healing tradition which is based on the concept that qi (life’s vital force) and xue (blood) surge through the body.
An imbalance in qi is thought to be caused by alterations in two opposite but complementary forces; yin and yang. Restoring balance requires achieving equilibrium between one’s internal organs and the external elements of earth, water, fire, wood and metal.
Certification in TCM requires 3 to 4 years of post-graduate study in the USA at an accredited TCM institution.
TCM treatment utilizes three main components: acupuncture, the mind–body interventions of tai chi and qi gong and also herbal products.
Acupuncture involves inserting thin needles into the body following meridians or energy circuits along which qi flows. In Parkinson’s disease, randomized controlled trials studying motor outcomes have yielded mixed results. Trials evaluating non-motor symptoms have shown more promising improvements in depression, anxiety, sleep, pain, fatigue, dysphagia and quality of life. Trial methodology can be challenging, and sham acupuncture has been shown to yield positive results in a few recent studies.
Tai chi is a Chinese martial art that combines deep breathing and disciplined movements to integrate balance, flexibility and meditative awareness.
Tai Chi has been studied extensively in Parkinson’s disease and there is a strong evidence base for improvements in gait, balance and falls.
Like Tai Chi, Qi Gong also incorporates movement, breathing, posture and meditation to enhance the flow of qi. Qi Gong has not in studies to date led to significant improvements in motor function, balance or fall reduction in randomized controlled trials. Sleep may also possibly be improved with Qi Gong.
Indigenous Medicine
Traditional Indigenous medicine is a holistic, ecologically based system centered on the belief that Mother Earth is the life source that interconnects humans, our ancestors and the environment.
Reverence and gratitude for all planetary relationships should guide the responsibility to preserve all life.
Indigenous healing highlights the need for balance between the body, mind, spirit, nature and the land beneath us.
We are hopeful studies will be performed in this area to see how this practice of medicine will impact Parkinson’s disease.
Having trouble accessing opportunities? When accessibility is a concern, utilize free online Yoga, Tai Chi, and Gi Gong classes. Several websites and mobile applications actually offer free guided meditations and breathing exercises.
What about mind–body strategies?
In addition to the mind–body interventions discussed above, we would add that expressive therapies have also been studied in Parkinson’s disease. We classify these therapies under mind–body strategies since they can help people disconnect from their surroundings and enter into a flow state.
Expressive therapies may be more accessible than traditional meditation or yoga.
Art Therapy
Nice piece by Drug Discovery news on prescribing art therapy for Parkinson’s disease.
Art therapy can address the frequently under-recognized visuospatial deficits in persons with Parkinson’s disease. These hidden challenges can consist of abnormal contrast sensitivity, color discrimination, dark–light adaptation, visual recognition and impairment in conjugate eye movements. Two recent trials using art therapy showed improvement in visual-cognitive skills, visuospatial processing and also improvement in overall motor function.
Art therapy is excellent for persons with Parkinson’s disease to improve mood, social connection and to enhance meaning of life, however this area is less studied.
Music Therapy
Music therapy augments movement and expression in order to meet physical, cognitive, psychological or social needs.
Studies of music have demonstrated improvements in Parkinson’s gait speed, stride length, cadence and motor coordination. The benefits of music therapy are thought to be due to modulation of internal rhythmic cueing.
Two recent studies, one combining treadmill walking with music and a second combining home-based gait training with a metronome, were found to improve gait performance and to reduce falls. There were two randomized controlled trials exploring drum playing along with rhythmic auditory stimulation and these both showed improvement in upper extremity motor function and attention.
Music therapy is a safe and enjoyable rehabilitation technique that is also well-received in group settings.
Finally, there was one study that showed listening to the Bee Gee’s when walking outperformed a metronome (University of Florida). Get your groove on.
Dance Therapy
Great article by Ina Jaffe at NPR in 2016 on Dance for Parkinson’s disease.
Dance therapy uses both movement and music to support the body’s physical, emotional, cognitive and social well-being.
The main goals of dance therapy are usually focused on: greater postural stability, improved balance, reintegration into a community, creative expression, enhanced body awareness, motor coordination and relaxation.
Many studies have shown various levels of improvement in gait, balance, mobility, and cognition in Parkinson’s disease. There are a lot of studies on some dances like the Tango.
There was a randomized controlled trial of Argentine tango vs. Tai Chi and though both improved symptoms, one was not better than the other.
Dance for Parkinson’s disease has been shown to improve self-esteem and quality of life.
In one study a dance-physiotherapy combined intervention was found to be safe, well-tolerated, and more effective than conventional physiotherapy alone in reducing motor dysfunction in Parkinson’s disease.
There are many dance programs for PD and one of the most famous is the Mark Morris Group led by David Leventhal (Dance for PD®)
Look for dance groups in your area that may or may not be affiliated with Mark Morris. There may be virtual and in-person classes across the globe for people of all abilities.
Culturally accessible practices are great when available.
Can we ‘integrate’ integrative medicine into our Parkinson’s disease programs?
You bet we can. Integrative medicine fits hand in glove with comprehensive multidisciplinary care for Parkinson’s disease. We challenge you to integrate as many principles as possible.
This blog was written by Indu Subramanian MD who is a co-editor of the parkinsonsecrets.com website and a movement disorders and integrative medicine specialist.
Pictured on the left is parkinsonsecrets.com artist Jonny Acheson and on the right website co-editor Michael S. Okun
Selected Recent References:
Kola S, Subramanian I. Updates in Parkinson's Disease Integrative Therapies: an Evidence-Based Review. Curr Neurol Neurosci Rep. 2023 Nov 3. doi: 10.1007/s11910-023-01312-z. Epub ahead of print. PMID: 37921943.
Li Q, Wu C, Wang X, Li Z, Hao X, Zhao L, Li M, Zhu M. Effect of acupuncture for non-motor symptoms in patients with Parkinson's disease: A systematic review and meta-analysis. Front Aging Neurosci. 2022 Oct 6;14:995850. doi: 10.3389/fnagi.2022.995850. PMID: 36275001; PMCID: PMC9582755.
Hanff AM, Leist AK, Fritz JV, Pauly C, Krüger R, Halek M; NCER-PD Consortium. Determinants of Self-Stigma in People with Parkinson's Disease: A Mixed Methods Scoping Review. J Parkinsons Dis. 2022;12(2):509-522. doi: 10.3233/JPD-212869. PMID: 34842199; PMCID: PMC8925108.
Ernst M, Folkerts AK, Gollan R, Lieker E, Caro-Valenzuela J, Adams A, Cryns N, Monsef I, Dresen A, Roheger M, Eggers C, Skoetz N, Kalbe E. Physical exercise for people with Parkinson's disease: a systematic review and network meta-analysis. Cochrane Database Syst Rev. 2023 Jan 5;1(1):CD013856. doi: 10.1002/14651858.CD013856.pub2. PMID: 36602886; PMCID: PMC9815433.
Solch RJ, Aigbogun JO, Voyiadjis AG, Talkington GM, Darensbourg RM, O'Connell S, Pickett KM, Perez SR, Maraganore DM. Mediterranean diet adherence, gut microbiota, and Alzheimer's or Parkinson's disease risk: A systematic review. J Neurol Sci. 2022 Mar 15;434:120166. doi: 10.1016/j.jns.2022.120166. Epub 2022 Jan 26. PMID: 35144237.
Thangaleela S, Sivamaruthi BS, Kesika P, Chaiyasut C. Role of Probiotics and Diet in the Management of Neurological Diseases and Mood States: A Review. Microorganisms. 2022 Nov 15;10(11):2268. doi: 10.3390/microorganisms10112268. PMID: 36422338; PMCID: PMC9696277.