Quaking our way to a Parkinson's biomarker breakthrough in 2023?
By Michael S. Okun M.D.
The news of a significant breakthrough in the development of a Parkinson’s disease biomarker spread at near hypersonic speed and it generated a ton of excitement in the field. What does it all mean? What is this biomarker and where did it come from? Will it affect me if I have Parkinson’s disease? How will it influence our search for new Parkinson’s therapies? Did you know the real breakthrough was in 2008-2016 as the methods for seeding assays were developed for another disease (Creutzfeldt-Jakob disease, prion). I will address all of these questions and more in the wake of the announcement of a biomarker for Parkinson’s disease in this month’s parkinsonsecrets.com blog.
What is the 2023 Parkinson’s disease biomarker breakthrough I keep hearing about?
On April 12, 2023 the Michael J. Fox Foundation for Parkinson’s Disease Research announced in a press release that researchers working on a project called PPMI had published an important paper in Lancet Neurology.
This is the Lancet Neurology 2023 paper which applied the synuclein seeding assay for Parkinson’s disease to the ~1000 subjects enrolled in the PPMI cohort.
The Michael J. Fox Foundation for Parkinson’s Disease Research should be given a lot of credit for pioneering a study called the Parkinson’s Progression Marker Initiative or PPMI. In this study, many researchers and clinicians from around the world have been depositing data about folks living with Parkinson’s, folks without Parkinson’s and folks who may be at risk to develop Parkinson’s disease. The data included details on specific symptoms, and also included deposits of a ‘fluid’ which bathes the brain and spinal cord (cerebrospinal fluid or spinal fluid). The foundation collected information on the presence of any Parkinson’s genes, any abnormalities on smell testing, and the presence of sleep disorders, such as REM sleep behavioral disorder. The ‘biomarker breakthrough’ occurred when the investigators from the study applied a technique to the collected spinal fluid called RT-QuIC in the form of a synuclein seeding assay. Their aim was to detect a protein called ‘synuclein;’ one of the suspects implicated in the Parkinson’s disease process. The study lead author was Andrew Siderowf from the University of Pennsylvania and the study senior author was Claudio Soto; Soto was a pioneer in developing the ‘synuclein seeding assay.’ Many other authors participated and contributed samples, data and expertise including a prominent contribution from Ken Marek (from the Michael J. Fox Foundation).
What is the ‘synuclein seeding’ biomarker assay and where did it come from?
In a 2020 article Candalise oulined how RT-QuIC would influence not only prion diagnosis but also degenerative disease diagnosis such as Parkinson’s and Alzheimer’s.
Here is the shocker contained in this month’s blog:
The RT-QuIC analysis, which is a key component of the synuclein seeding assay, was designed as a diagnostic test for prion disease (Creutzfeldt-Jakob disease or CJD), and not for Parkinson’s disease. This extended application is another shining example of how scientific breakthroughs can be multiplied when applied across diseases.
The pathological hallmark of of CJD is referred to as the prion protein or PrPSc. There are very small amounts of this ‘biomarker’ protein found in samples of cerebrospinal fluid, and when investigators tried to develop antibodies against the protein, they kept detecting normal, as well as abnormal PrPSc.
In 2010 the problem was ‘solved’ when real-time quaking-induced conversion (RT-QuIC) was introduced. In a brilliant new method, scientists took cerebrospinal fluid of a CJD patient and mixed it with a version of PrP called recombinant PrP; they also mixed it with a substance called thioflavin T.
The fluid was then ‘quaked’ by a machine (shaken) for many hours. Scientists took suspected CJD fluid with ‘bad misfolded prion protein’ and showed when quaked it could induce misfolding and aggregation of the normal recombinant prion protein (which was mixed together). Simply put, the bad protein (PrPSc) binds to the good recombinant PrP.
This reaction induced a change in its shape and also the formation of ‘crystalized’ fibrils. Fibrils clump, bind thioflavin T, and glow. When this occurred it was a eureka moment as it became obvious the sample was infected with CJD.
Now you know where the method gets it’s name:
Real-time quaking-induced conversion (RT-QuIC) which is part of a process to perform a synuclein seeding assay.
Alison Green nicely summarizes the history of RT-QuIC and how it was introduced as a test for prion disease (CJD) in a 2019 article which appeared in Practical Neurology.
Nice paper in neurology showing how seeding assay work for Parkinson’s and multiple system atrophy (MSA). https://n.neurology.org/content/99/5/195 Notice in this picture it takes longer to see the changes in MSA.
Why do we call it a ‘seeding assay?’
This is from a Nature Protocols paper by Claudio Soto from 2023 and the picture details the methods of the ‘synuclein seeding’ assay. https://www.nature.com/articles/s41596-022-00787-3
Here are some simple steps to think about how a ‘seeding assay’ can be applied for Parkinson’s.
1- Imagine when you plant a seed it grows.
2- Now imagine if the ‘seed you plant’ is actually a sample of a body fluid (e.g. spinal fluid) which contains a bad (a pathological form called a misfolded oligomer) version of the Parkinson’s related protein (alpha synuclein).
3- You then drop in the ‘seed’ (which is actually the bad form of Parkinson’s protein) into a mixture which also contains the normal version of the protein (alpha synuclein).
4- You ‘quake’ or shake the mixture and the abnormal Parkinson’s protein converts some or all of the normal Parkinson’s protein into the pathological or ‘bad form of alpha synuclein.’ Also, as the process evolves, proteins tend form ‘crystalized fibrils’ which can be identified and quantified.
5- You measure (over time) this conversion of good protein into bad. You ‘mark’ the amount of ‘bad alpha synuclein protein’ using a tag that makes it glow (or alternatively by using an antibody). You are interested in how fast the conversion to bad alpha synuclein takes place. A faster conversion into pathological or bad alpha synuclein has been associated with Parkinson’s disease, and in contrast, a slower conversion has been demonstrated with another ‘synucleinopathy’ called multiple system atrophy (MSA).
Why do people refer to the behavior of the Parkinson’s related protein as prion-like?
Some of the early notions of ‘prion like spread’ were described in this Nature paper from 2009.
Many scientists have compared the mechanism of spread of CJD (prion disease) to the mechanism of the spread of Parkinson’s disease within the brain and the nervous system. There is much debate about this topic, however the idea that ‘misfolded Parkinson’s disease proteins’ can spread throughout the brain (like a prion) has been referred to as ‘prion-like behavior.’ The cool angle to this story is that research in prion diseases actually triggered the development of the current seeding assays used for Parkinson’s disease.
Un Kang and colleagues at NYU, in a recent paper (2019) published in Movement Disorders, compared a few RT-QuIC synuclein assays and further explained the process of ‘seeding.’
The alpha synuclein protein is part of the ‘depositions’ which appear in Parkinson’s disease brains ; we frequently refer to these as Lewy bodies. We take advantage of the different shapes of alpha synuclein and how alpha synuclein folds into different configurations. The ‘oligomer’ configuration of alpha synuclein promotes aggregation. Some experts in Parkinson’s disease refer to these ‘pathologic’ oligomers as prion-like, because they seem to spread throughout the brain, similar to what would be observed in an infectious disease.
The abnormal configuration of alpha synuclein can ‘propagate or spread’ its abnormal conformation to normal alpha synuclein. We take full advantage of this behavior of alpha synuclein to diagnose Parkinson’s disease using the seeding assays. Thus, we can thank CJD researchers for catapulting Parkinson’s disease biomarker research to a new level.
Spoiler alert: Not all Parkinson’s ‘synuclein assays’ are equal and we must pay attention to the methods used and we must keep ‘perfecting’ the technique.
What discoveries contributed to synuclein seeding assays?
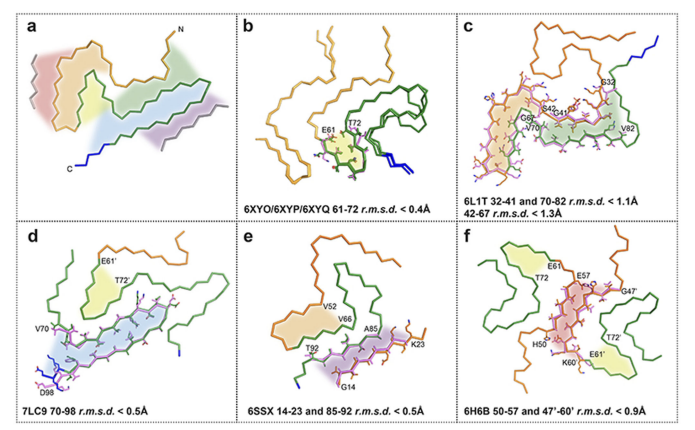
The story of the development of the alpha synuclein biomarker for Parkinson’s disease began with seminal discoveries in seeding and the use of a technique called RT-QuIC. Many experts refer to these tests collectively as seed amplification assays (SAAs). These assays can (incredibly) detect minimal amounts of ‘abnormal protein.’ Scientists have used SAA fluorescence profiles or ‘glowing’ to identify the abnormal synuclein fibril conformations.
One of the fathers of the science behind seeding whose work significantly contributed to the development and use of RT-QuIC and later synuclein seeding assays was Claudio Soto. You may notice his name as he is the senior author of the recently published Lancet neurology paper which applied his technique to the PPMI cohort. There are however also many other important scientists in the development of seeding and RT-QuIC including Alison Green, Byron Caughey, Ryuichiro Atarashi and others.
Guess what? Researchers have been quaking samples since the early 2000’s and by 2010 they had perfected the test for prion (CJD disease). One example of this early work is a nice article from Nature Methods in 2008.
Who gets the credit for RT- QuIC and synuclein assays for prion and Parkinson’s?
Who first applied RT-QuIC to synucleinopathies and to Parkinson’s disease?'
Many people believe the earliest work on seeding can be credited to Claudio Soto. In fact a form of Soto’s assay was the one used for the most recent article which appeared in Lancet Neurology on the PPMI cohort.
It is however always hard to judge ‘who used it first in Parkinson’s, however most experts cite the Fairfoul and Green paper in 2016 and the Groveman paper in 2018 as pioneering work in RT-QuIC for Parkinson’s disease. By 2018 Sano and Nishida and a slew of other laboratories had become part of the RT-QuIC revolution for diagnosis in Parkinson’s disease.
Selected Publications on Seeding, RT-QuIC and Parkinson’s:
Fairfoul G, McGuire LI, Pal S, Ironside JW, Neumann J, Christie S, Joachim C, Esiri M, Evetts SG, Rolinski M, Baig F, Ruffmann C, Wade-Martins R, Hu MT, Parkkinen L, Green AJ. Alpha-synuclein RT-QuIC in the CSF of patients with alpha-synucleinopathies. Ann Clin Transl Neurol. 2016 Aug 28;3(10):812-818. doi: 10.1002/acn3.338. PMID: 27752516; PMCID: PMC5048391.
Groveman BR, Orrù CD, Hughson AG, Raymond LD, Zanusso G, Ghetti B, Campbell KJ, Safar J, Galasko D, Caughey B. Rapid and ultra-sensitive quantitation of disease-associated α-synuclein seeds in brain and cerebrospinal fluid by αSyn RT-QuIC. Acta Neuropathol Commun. 2018 Feb 9;6(1):7. doi: 10.1186/s40478-018-0508-2. Erratum in: Acta Neuropathol Commun. 2020 Nov 5;8(1):180. PMID: 29422107; PMCID: PMC5806364.
Sano K, Atarashi R, Satoh K, Ishibashi D, Nakagaki T, Iwasaki Y, Yoshida M, Murayama S, Mishima K, Nishida N. Prion-Like Seeding of Misfolded α-Synuclein in the Brains of Dementia with Lewy Body Patients in RT-QUIC. Mol Neurobiol. 2018 May;55(5):3916-3930. doi: 10.1007/s12035-017-0624-1. Epub 2017 May 26. PMID: 28550528; PMCID: PMC5884914.14. Fairfoul G, et al. Alpha-synuclein RT-QuIC in the CSF of patients with alpha-synucleinopathies. Ann. Clin. Transl. Neurol. 2016;3:812–818. [PMC free article] [PubMed] [Google Scholar]
What did the Lancet Neurology paper show in 2023 on seeding in Parkinson’s?
Data from the PPMI seed assay Lancet paper in 2023 showed the differences in sporadic, LRRK2 and GBA Parkinson’s disease.
Here are the key takeaway points from the 2023 article on the PPMI cohort and the SAA assay.:
The data was cross sectional and included sporadic Parkinson's disease, healthy controls, and prodromal rapid eye movement sleep behavior disorder or hyposmia.
They also tested non-manifesting carriers of LRRK2 and GBA variants.
The sensitivity for Parkinson's disease diagnosis was 87.7% and specificity for healthy controls was 96.3%.
The sensitivity of the α-synuclein SAA assay in Parkinson's disease when they included the characteristic of anosmia improved to 98.6%.
The α-synuclein (SAA) assay did not perform as well in LRRK2 Parkinson's disease (67.5%) and in sporadic Parkinson's disease without anosmia (78.3%).
In prodromal and at-risk groups, 86% had a positive α-synuclein SAA. There were only 8% of non-manifesting carriers who had a positive assay.
There was a gender difference in results for women in this study and that data will need to be followed up as it may offer us an important insight into Parkinson’s disease.
What do we need to improve on as we chart a path forward for synuclein assays?
We must recognize that the alpha synuclein SAA biomarker for possible Parkinson’s disease is not perfect and is just one of many assays in development. There is room for ‘much improvement.’
The data was cross-sectional and not longitudinal, and therefore longer-term data will be helpful to guide the field.
A key importance of the data from the current study is that it was applied to a very large group of patients, however all biomarker studies will at some point need an independent replication cohort so we can be sure of the findings.
The study used cerebrospinal fluid. and ideally we will need more practical sources of biologicals so that one day soon we can offer access to this test across all geographies and economies (e.g. use of skin or blood for example would be ideal).
Many previous authors have shown that the methodology of RT-QuIC and seed assays MATTERS. Results can vary by 40-50% depending on the quality of the assay. We need to keep this challenge ‘top of mind.’
The authors of the Lancet paper used a technique designed by Claudio Soto that was commercialized into a company product. We need to be sure we keep improve the quality of this test (and other tests).
Though this study lacked an independent validation cohort, the results, including the lower rate of positivity in the LRRK2 population, match previously published studies. This is an area experts will need to better understand.
Will the availability of new ‘synuclein seeding assays’ for Parkinson’s disease diagnosis alter my current disease management?
The short answer is no. Here are some bottom line take home points if you are a person with Parkinson’s disease and areas we can pursue:
The identification of biomarkers for diagnosis (and to follow disease progression) in Parkinson’s disease will be important for the field as it moves forward.
If you have dopamine responsive Parkinson’s disease it is unlikely that this new assay will immediately alter your treatment in any meaningful way. In fact, rushing out to get the test if you already have Parkinson’s and you are under treatment, may lead to confusion if it is negative (like what was seen in a large percentage of folks with the LRRK2 mutation in the Lancet Neurology study).
Volunteering to have the assay performed for research and for inclusion into clinical trials will be an important new use for this test. We highly encourage you to volunteer for studies.
This assay (and potentially others) will help us to build a better classification system for Parkinson’s disease, so that we can work more effectively with the FDA and other regulatory agencies to fast-track the development new Parkinson’s therapies.
It is important to understand that the assay amplifies the signal of an alpha synuclein containing tissue and this finding is not a direct reflection of what is going on in the brain; thus the assay probably does not represent a complete picture of the underlying pathophysiology of Parkinson’s disease.
Parkinson’s disease is not ‘one disease’ and that is a challenge for this biomarker assay and for any future biomarker assays. Additionally, this assay focuses on aggregated abnormal protein and not on the normal protein and quantifying normal protein could also be important in the future.
Creating a ‘future’ biological definition for Parkinson’s disease will be challenging and it should include input from clinicians, scientists and most important from persons with Parkinson’s disease. We should anticipate the efforts for creating new biological definitions to rapidly proceed in the wake of the the ‘synuclein assay era.’
Michael Okun is the author of this blog post and along with Dr. Indu Subramanian provides content for parkinsonsecrets.com
Jonny Acheson is the website artist and also is a doctor and person with Parkinson’s disease.