An expert weighs in on the "top 5" updates in imaging and drug/device development in dystonia
There are so many exciting projects going on in dystonia research that it has become hard to keep up with all of the advances. We sat down with one of the worlds top dystonia and Parkinson imaging researchers (Dr. David Vaillancourt) to talk about the “top 5” updates in therapies and in dystonia imaging research.
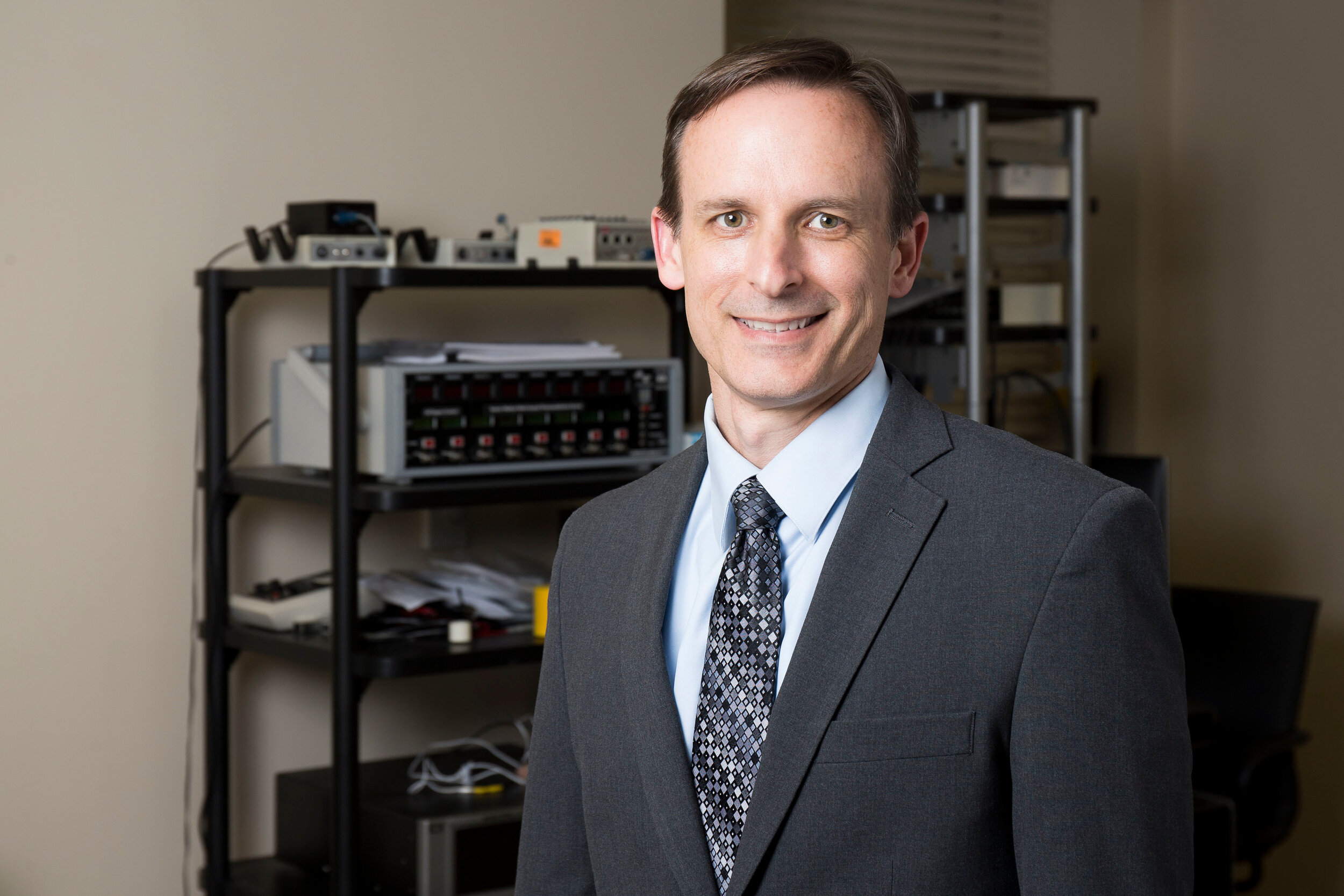
Who is David Vaillancourt?
David Vaillancourt is Chair and Professor in the Department of Applied Physiology and Kinesiology at the University of Florida.
He is funded by Tyler’s Hope for a Dystonia Cure to do cutting edge imaging research and he collaborates with UF researchers Yuquing Li and Marcelo Febo.
Yuquing Li, PhD., University of Florida
Vaillancourt’s research focuses on how the brain regulates voluntary and involuntary movement with a specific focus on motor disorders.
He uses advanced neuroimaging techniques to study the functional and structural changes in the brain of humans and animal models.
He has used rehabilitative, surgical, and pharmacological interventions, and published his work in journals including Brain, Journal of Neuroscience, JAMA Neurology, Neurology, Human Brain Mapping, Neuroimage, Cerebral Cortex, and Neurobiology of Aging.
He has been continuously funded by NIH since 1999, and now directs several grants from NIH.
In dystonia he studies the pharmacological and neuroimaging in mouse and human models.
Marcelo Febo, PhD., University of Florida
Dr. Vaillancourt’s Top 5 Updates in Imaging and
research into dystonia.
1) What is imaging and how is it used in dystonia?
Neuroimaging is a broad term. It encompasses imaging using positron emission tomography, magnetic resonance imaging, and other techniques. In positron emission tomography, the approach is to inject a drug or tracer into the blood stream. This drug or tracer can cross into the brain. The tracer is then imaged in an effort to measure how the neural receptors respond. This procedure can be useful in many ways because the tracer can be designed to be specific to the neural receptors in the brain.
In dystonia, the types of tracers that are mostly used are dopamine related tracers and cholinergic related tracers.
Other forms of imaging include functional magnetic resonance imaging and structural magnetic resonance imaging. These techniques examine how protons in water are affected by blood flow and tissue specific changes. These methods can help to pinpoint where in the brain dystonia can manifest and where in the brain specific new therapies should be targeted
2) What is a specific example in humans for how
imaging is being used in dystonia?
In a recent study published in the journal Brain (Corp et al. 2019; PMID: 31099831) the authors used a clever approach. They studied people with cervical dystonia who had lesions in the brain (e.g. strokes, tumors) causing the dystonia. Whereas most types of dystonia do not have a visual lesion on the MRI, these authors focused on rare patients with visible lesions on their brain scan. Next, they used a technique called resting state functional MRI to map a “connectome” type network that presumably links all of these brain regions together.
The authors observed that two regions of the brain were connected to all of the brain lesions across all of the patients with cervical dystonia. Thus there were common nodes of dysfunction possibly underpinning the cause(s) of the dystonia. The two regions— somatosensory cortex and the cerebellum— were found to link to all of the lesioned regions across all of the cervical dystonia patients. This new finding tells us two things:
1) It tells us that these two regions may be critical for therapies targeting dystonia; and
2) It tells us that studies in dystonia may consider targeting therapies directly to these parts of the brain or to their connections.
3) What is a specific example in animals for how
imaging is being used in dystonia?
The Calakos Laboratory at Duke University is working on new therapies to potentiallu help people with dystonia through a large alignment grant funded by Tyler’s Hope for a Dystonia Cure. Their work is focused on therapies that can target specific cellular pathways. They are focused on the eIF2alpha signaling pathway in DYT1 dystonia. In a recent paper (Rittiner et al. 2016; PMID: 27939583) the authors found that patient-derived cells and a mouse model both supported a pathogenic role for this pathway (e.g. it was likely involved in dystonia). The authors also found that this pathway had therapeutic potential and may help to develop a “drug-able” target.
Dr. Calakos is now working with Dr. Vaillancourt to test if a medication can be safely delivered to the brains of mice which are genetically similar to human DYT1 dystonia. We are using a high-field MRI that goes up to 17 Tesla (a typical MRI is 1.5-3 Tesla). The high-field MRI will provide enhanced signal for the tiny mouse brain so we can see the brain and the drug of interest.
The experiments will determine if the medication is affecting the brain tissue of the mouse. This type of experiment will help move us closer to a therapeutic for dystonia.
4) How can imaging be used in humans to assess a
new therapeutic (e.g. drug, device)?
If a therapeutic (e.g. drug, device) is deemed safe for humans, it can be further studied
The safety is typically assessed in a Phase 1 study, which will examine different dose levels of a medication and will determine which levels are safe. If a Phase 1 study is successful, the drug can move to a Phase 2 study where safety and other data readouts will be assessed (e.g. how well it works, what pathways does it affect). In the Phase 2 study, imaging methods can be used to determine where in the brain a medication is influencing the system.
In moving from a Phase 2 to a Phase 3 study, the investment for a device or pharmaceutical company can be significant, and thus the company will typically want to see several “readouts” that show the medication could will have the potential to work on the disease (e.g. dystonia).
5) What does this all mean for people with dystonia?
I believe that these issues means several things and here is my interpretation:
1) People care about you and care about dystonia. There are labs across the world working on dystonia. They are conducting studies in cells, live animals, and in human clinical trials.
2) Treatments take time to develop. The studies that I have mentioned, took years to complete. There are many other studies in the field of dystonia and even though this is a big effort, it takes time--it is 100% worth it.
3) Stay the course. In research, sometimes research does not have a positive outcome. It can take several years to find out you are “going down the wrong path.” However, sometimes research yields a breakthrough that can change how we treat a patient and improve their quality of life. This is what we hope for and strive for…so stay the course! We are optimistic we are making progress in imaging and dystonia drug/device research!
To read more books and articles by Michael S. Okun MD check Twitter @MichaelOkun and these websites with blogs and information on his blogs and books Dystonia Tips and Research @TylersHope #TylersHope #Dystoniasucks